I. Introduction
A. What is Health Information Exchange (HIE)?
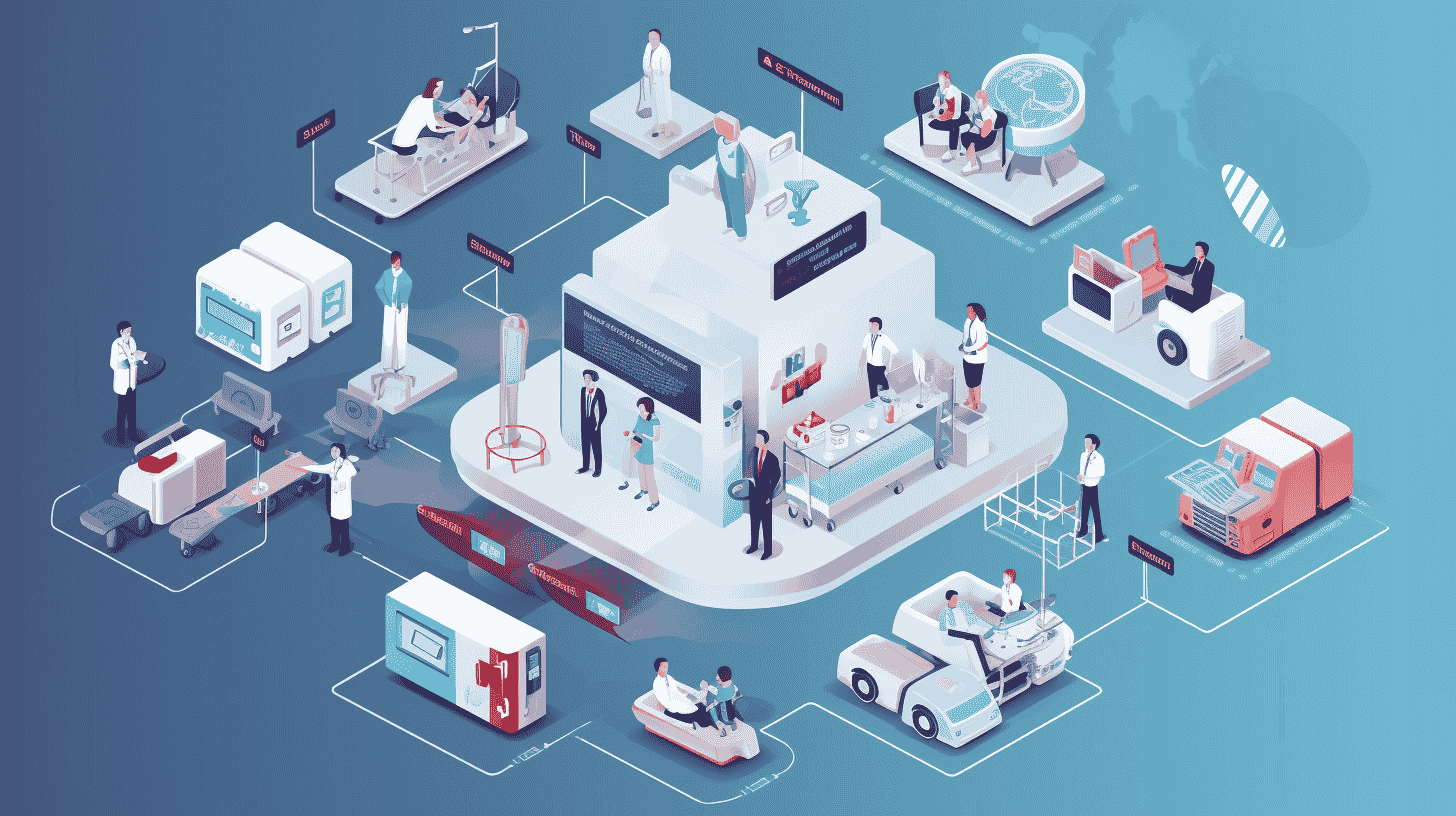
Health Information Exchange (HIE) refers to the electronic sharing of healthcare information among different healthcare organizations and systems. The goal of HIE is to facilitate the secure and efficient exchange of patient health information across various healthcare settings, such as hospitals, clinics, laboratories, pharmacies, and other healthcare providers. The primary aim is to improve the quality and coordination of patient care.
In traditional healthcare systems, patient information is often fragmented and stored in separate, isolated systems. This fragmentation can lead to inefficiencies, delays in treatment, and potential errors in patient care. HIE addresses these challenges by creating a framework for the electronic exchange of health information, allowing authorized healthcare professionals to access and share relevant patient data in a timely and secure manner.
B. How is Health Information Exchange used in healthcare?
Health Information Exchange (HIE) is used in healthcare to facilitate the seamless sharing of patient health information across various healthcare organizations and systems. Its implementation has several practical applications that contribute to improved patient care, increased efficiency, and better overall healthcare outcomes. Here are some key ways in which HIE is used in healthcare:
-
Improved Care Coordination:
- Access to Comprehensive Patient Records: HIE allows authorized healthcare providers to access a patient's comprehensive health record, including medical history, medications, allergies, test results, and treatment plans. This access enhances the ability of healthcare teams to coordinate and deliver more informed and personalized care.
-
Enhanced Decision-Making:
- Real-time Information: HIE provides real-time access to critical patient information, enabling healthcare professionals to make informed decisions promptly. This is particularly crucial in emergency situations or when patients receive care from multiple providers.
-
Reduction of Duplicate Tests and Procedures:
- Avoiding Redundancy: With HIE, healthcare providers can quickly retrieve a patient's medical history, reducing the need for duplicate tests and procedures. This not only saves time and resources but also minimizes unnecessary exposure to medical interventions.
-
Medication Management:
- Medication Reconciliation: HIE helps healthcare providers reconcile medications across different settings, reducing the risk of medication errors. This is especially important when patients receive care from multiple providers who may prescribe different medications.
-
Public Health Surveillance:
- Disease Monitoring and Reporting: HIE contributes to public health efforts by providing timely and accurate data for disease surveillance and reporting. This is valuable for tracking the spread of diseases, identifying outbreaks, and implementing appropriate public health interventions.
-
Patient Engagement:
- Access to Personal Health Information: Patients can benefit from HIE by having better access to their own health information. This can empower individuals to be more engaged in their healthcare decisions and to actively participate in managing their health.
-
Efficient Referral Processes:
- Streamlined Referrals: HIE streamlines the referral process by allowing referring and receiving healthcare providers to share relevant patient information efficiently. This ensures continuity of care and a smoother transition between different levels of healthcare.
-
Reduced Administrative Burden:
- Streamlined Administrative Processes: HIE helps reduce administrative burdens by automating the exchange of information. This can lead to improved workflow efficiency for healthcare organizations.
-
Research and Population Health Management:
- Data for Research Purposes: Aggregated and de-identified data from HIE can be used for research purposes, contributing to population health management initiatives and the development of evidence-based healthcare practices.
C. Brief overview of the evolution of HIE
The evolution of Health Information Exchange (HIE) can be traced through several key stages, each marked by technological advancements, policy changes, and a growing recognition of the importance of seamless information sharing in healthcare. Here is a brief overview of the evolution of HIE:
-
Paper-Based Systems:
- In the early days of healthcare, patient information was recorded and stored on paper. This manual process was time-consuming, prone to errors, and made it challenging to share information across different healthcare providers and facilities.
-
Emergence of Electronic Health Records (EHRs):
- The transition to electronic health records marked a significant advancement. EHRs digitized patient information, making it more accessible within a single healthcare organization. However, interoperability challenges persisted, limiting the exchange of information across different systems.
-
Regional Health Information Organizations (RHIOs):
- Recognizing the need for broader information exchange, the concept of Regional Health Information Organizations (RHIOs) emerged. These were regional entities that aimed to facilitate the sharing of health information among healthcare providers within a specific geographic area. RHIOs played a crucial role in laying the groundwork for broader HIE initiatives.
-
Government Initiatives and Funding:
- Governments, particularly in the United States with the passage of the Health Information Technology for Economic and Clinical Health (HITECH) Act in 2009, began actively promoting the adoption of electronic health records and HIE. Financial incentives were provided to encourage healthcare organizations to implement interoperable systems.
-
National Health Information Network (NHIN):
- The concept of a National Health Information Network (NHIN) emerged as a vision for a nationwide health information exchange. The NHIN aimed to create a framework for secure and interoperable information exchange across the entire healthcare ecosystem.
-
Advancements in Interoperability Standards:
- As technology evolved, there was a focus on developing and adopting interoperability standards. Standards, such as Health Level Seven International (HL7) and Fast Healthcare Interoperability Resources (FHIR), played a crucial role in ensuring that different health IT systems could communicate effectively.
-
Expansion of HIE Networks:
- HIE networks continued to expand, connecting healthcare providers and organizations within and across regions. This expansion facilitated the exchange of patient information on a broader scale, improving care coordination and patient outcomes.
-
Increased Emphasis on Privacy and Security:
- With the growing exchange of sensitive health information, there was an increased emphasis on privacy and security measures. Strict regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), set guidelines for safeguarding patient data during exchange.
-
Technological Advancements and Cloud-Based Solutions:
- Technological advancements, including the widespread adoption of cloud computing, contributed to more scalable and flexible HIE solutions. Cloud-based platforms allowed for easier data sharing and collaboration among healthcare entities.
-
Focus on Patient-Centered Care:
- More recently, there has been a shift towards patient-centered care, emphasizing the importance of involving patients in the management of their health information. Patient portals and tools for accessing personal health records contribute to this evolution.
-
Interconnected Health Ecosystem:
- The vision for HIE is evolving towards creating an interconnected health ecosystem where information seamlessly flows between patients, healthcare providers, payers, and public health agencies. This interconnectedness is essential for achieving truly coordinated and personalized healthcare.
II. The Need for Health Information Exchange
A. Challenges in traditional healthcare information systems
Traditional healthcare information systems, often relying on paper-based or legacy electronic systems, face several challenges that impact the efficiency, accuracy, and accessibility of healthcare data. Some of the key challenges include:
-
Fragmentation of Data:
- Traditional systems often lead to fragmented and siloed data, where patient information is stored in disparate formats and locations. This makes it difficult for healthcare providers to access a comprehensive view of a patient's medical history.
-
Limited Interoperability:
- Lack of interoperability among different healthcare information systems is a significant challenge. Incompatibility between systems hinders the seamless exchange of information, making it challenging for healthcare providers to share and access patient data across different settings.
-
Data Inaccuracy and Duplication:
- Manual data entry in paper-based systems or outdated electronic systems can lead to errors and inaccuracies in patient records. Duplication of data entry across multiple systems may result in inconsistencies and confusion.
-
Security and Privacy Concerns:
- Paper records and older electronic systems may not have robust security measures in place to protect patient information. This poses a risk of unauthorized access, data breaches, and compromises to patient privacy.
-
Limited Accessibility and Timeliness:
- Retrieving patient information from paper records or legacy systems can be time-consuming. In emergency situations, delays in accessing critical information can impact the speed and effectiveness of patient care.
-
Resistance to Change:
- Healthcare professionals may resist transitioning from familiar but outdated systems to newer technologies. Resistance to change can slow down the adoption of more efficient and interconnected healthcare information systems.
-
Inefficient Workflow and Administrative Burden:
- Traditional systems may contribute to inefficient workflows, with healthcare providers spending excessive time on administrative tasks such as manual data entry, retrieval of paper records, and coordination between different departments.
-
Limited Patient Engagement:
- Traditional systems often do not provide easy access to health information for patients. This limits patient engagement and empowerment, as individuals may have limited control over their own health data.
-
Scalability Issues:
- Traditional systems may struggle to scale effectively with the growing volume of healthcare data and the increasing complexity of healthcare delivery. This can result in inadequate support for evolving healthcare needs.
-
Regulatory Compliance Challenges:
- Compliance with evolving healthcare regulations, such as those related to privacy and security (e.g., HIPAA), can be challenging for traditional systems that may not have built-in features to address these requirements.
-
High Costs of Maintenance:
- Maintaining and upgrading legacy systems can be expensive. The costs associated with keeping outdated systems operational may divert resources that could be better utilized for implementing more modern and efficient healthcare information systems.
B. Importance of timely and accurate information in patient care
In the context of Health Information Exchange (HIE), the importance of timely and accurate information in patient care cannot be overstated. HIE facilitates the seamless sharing of health information across different healthcare entities, ensuring that relevant and up-to-date patient data is readily available to healthcare providers when needed. Timely access to information through HIE is particularly critical in emergency situations, allowing healthcare professionals to make swift and well-informed decisions that can significantly impact patient outcomes. Moreover, accurate information exchanged through HIE helps prevent medical errors, supports effective care coordination among various providers, and contributes to a more comprehensive understanding of a patient's health history. By streamlining the exchange of timely and accurate information, HIE enhances the efficiency of healthcare delivery, reduces redundant tests and procedures, and ultimately leads to improved patient care and safety.
C. How many forms of Health Information Exchange (HIE) are there?
Health Information Exchange (HIE) can take various forms, each with its unique characteristics and purposes. While the specific models and terminology may vary, here are some common forms of HIE:
-
Directed Exchange:
- In directed exchange, healthcare providers and organizations electronically send patient information directly to known and authorized recipients, such as referring physicians or specialists. This form is often used for specific care coordination purposes.
-
Query-Based Exchange:
- Query-based exchange allows healthcare providers to request and retrieve patient information from other providers or entities. This on-demand model enables healthcare professionals to access relevant data when needed for patient care.
-
Consumer-Mediated Exchange:
- In consumer-mediated exchange, patients have a more active role in managing and sharing their health information. Patients can control access to their records and share them with healthcare providers or other entities through secure portals or applications.
-
Health Information Service Providers (HISP):
- HISPs facilitate secure messaging and data exchange between healthcare organizations. They play a role in ensuring the confidentiality and integrity of health information during transmission.
-
Community-Based Exchange:
- Community-based exchange involves the sharing of health information among healthcare providers within a specific geographic community or network. Regional Health Information Organizations (RHIOs) often facilitate community-based exchange.
-
Enterprise HIE:
- Enterprise HIE focuses on data exchange within a specific healthcare organization or enterprise. It enables different departments or entities within the organization to share patient information seamlessly.
-
Statewide HIE:
- Statewide HIE initiatives aim to connect healthcare organizations and providers across an entire state. These initiatives facilitate the exchange of health information on a broader scale, supporting care coordination and public health efforts.
-
National HIE:
- National HIE initiatives aspire to create a network that spans across the entire country, enabling the exchange of health information on a national level. The goal is to promote interoperability and data exchange among diverse healthcare entities.
-
Intermediary HIE Models:
- Some HIE models involve intermediaries or third-party organizations that facilitate the exchange of health information between healthcare entities. These intermediaries may aggregate, normalize, and transmit data on behalf of participating organizations.
-
Public Health Information Exchange:
- Public health information exchange involves the sharing of health data for public health purposes, such as disease surveillance, monitoring of health trends, and response to public health emergencies.
These forms of HIE may coexist within a healthcare ecosystem, and organizations may participate in multiple models to meet various needs. The choice of HIE model often depends on factors such as the scope of data exchange, the geographic reach of the network, and the specific goals of the participating entities.

III. How Health Information Exchange Works
A. Overview of the technical infrastructure of HIE
The technical infrastructure of Health Information Exchange (HIE) is a complex system designed to facilitate the secure and seamless exchange of health information among different healthcare entities. Several key components make up the technical framework of HIE:
-
Health Information Systems (HIS): HIE relies on a variety of health information systems, including Electronic Health Records (EHRs), Laboratory Information Systems (LIS), Radiology Information Systems (RIS), and Pharmacy Information Systems. These systems capture and store patient data in electronic formats.
-
Interoperability Standards: HIE systems adhere to interoperability standards that define how different health information systems communicate and share data. Standards such as Health Level Seven International (HL7) and Fast Healthcare Interoperability Resources (FHIR) play a crucial role in ensuring compatibility between diverse systems.
-
Health Information Exchange Platform (HIEP): At the core of HIE's technical infrastructure is the HIE platform itself. This platform serves as the centralized hub where data exchange occurs. It manages data routing, ensures data integrity, and provides the necessary security measures for protecting sensitive health information.
-
Data Aggregation and Normalization: HIE systems aggregate data from disparate sources and normalize it to a standardized format. This process ensures consistency and coherence, allowing healthcare providers to access a unified and comprehensive view of patient information.
-
Master Patient Index (MPI): The MPI is a critical component that helps uniquely identify and match patient records across different systems. It prevents duplication and ensures that healthcare providers retrieve accurate and complete patient information.
-
Security Infrastructure: Given the sensitivity of health information, robust security measures are integrated into HIE systems. This includes encryption, authentication protocols, and audit trails to protect patient privacy and comply with healthcare regulations like the Health Insurance Portability and Accountability Act (HIPAA).
-
Consent Management Systems: HIE often includes mechanisms for managing patient consent regarding the sharing of their health information. Consent management systems ensure that data is exchanged only with the explicit permission of the patient.
-
Health Information Service Providers (HISP): HISPs play a role in secure messaging within HIE systems. They enable the encrypted transmission of health information between different healthcare organizations, ensuring the confidentiality and integrity of the data in transit.
-
Directory Services: Directory services help in the discovery of where patient information is stored and who has access to it within the HIE network. This component is crucial for efficient and targeted data retrieval.
-
Audit and Reporting Systems: To maintain accountability and track data usage, HIE systems incorporate audit and reporting functionalities. These features enable monitoring of who accesses patient information and when, contributing to compliance and transparency.
-
Patient Portals: Some HIE systems include patient portals that empower individuals to access and manage their own health information. Patient engagement is increasingly recognized as an integral part of the technical infrastructure to promote a patient-centered approach.
B. Interoperability and standards in HIE
-
Interoperability:
- Definition: Interoperability in the context of HIE refers to the ability of diverse health information systems and applications to exchange, interpret, and use data cohesively.
- Types of Interoperability:
- Technical Interoperability: This involves the exchange of data between different systems and technologies. It ensures that systems can understand and use the information shared.
- Semantic Interoperability: This addresses the common understanding of the exchanged data. It ensures that the meaning of the information is preserved across different systems.
- Organizational Interoperability: This pertains to the coordination and alignment of policies, procedures, and workflows across different healthcare organizations to facilitate effective data exchange.
-
Standards:
- Definition: Standards in HIE refer to agreed-upon rules, conventions, or guidelines that facilitate uniformity and consistency in the way data is structured, transmitted, and interpreted.
- Types of Standards:
- Data Standards: Specify the format and structure of data, ensuring that information is represented consistently across different systems. Examples include HL7 (Health Level Seven) and CDA (Clinical Document Architecture).
- Communication Standards: Define the protocols and methods for transmitting data between systems. Examples include DICOM (Digital Imaging and Communications in Medicine) for medical imaging and IHE (Integrating the Healthcare Enterprise) profiles.
- Terminology Standards: Ensure consistent language and coding for clinical terms. SNOMED CT (Systematized Nomenclature of Medicine—Clinical Terms) and LOINC (Logical Observation Identifiers Names and Codes) are examples.
- Security Standards: Address the safeguarding of health information during transmission and storage, following regulations such as HIPAA (Health Insurance Portability and Accountability Act).
C. Key stakeholders involved in the HIE process
Health Information Exchange (HIE) involves collaboration among various stakeholders who play distinct roles in facilitating the seamless exchange of health information. Here are key stakeholders involved in the HIE process:
-
Healthcare Providers:
- Physicians, Nurses, and Allied Health Professionals: These frontline healthcare professionals actively use and contribute to the HIE system, accessing patient information to make informed decisions and provide timely care.
-
Healthcare Organizations:
- Hospitals, Clinics, and Medical Practices: These entities are central to the HIE process as they contribute to and retrieve patient data. The adoption of HIE within these organizations is essential for the success of information exchange initiatives.
-
Health Information Exchange Organizations:
- HIE Networks and Platforms: These entities operate and manage the technical infrastructure that facilitates the exchange of health information. They provide the framework for secure data transmission and storage.
-
Payers:
- Health Insurance Companies and Payer Organizations: Payers can benefit from HIE by accessing relevant patient data for claims processing, ensuring accurate billing, and supporting population health management initiatives.
-
Patients:
- Individuals and Patient Advocacy Groups: Patients play a crucial role in HIE by providing consent for the sharing of their health information. Patient engagement is increasingly emphasized, and some HIE systems offer individuals access to their own health records.
-
Government and Regulatory Bodies:
- Department of Health and Human Services (HHS), Office of the National Coordinator for Health IT (ONC): Government agencies set policies, regulations, and standards that influence HIE initiatives. In the United States, the ONC plays a key role in promoting interoperability and HIE.
-
Interoperability Standards Organizations:
- HL7 (Health Level Seven), IHE (Integrating the Healthcare Enterprise): These organizations develop and promote standards that facilitate interoperability in health information systems. Adherence to these standards is essential for seamless data exchange.
-
Technology Vendors:
- Electronic Health Record (EHR) Providers, Health IT Companies: Technology vendors develop and provide the software and systems that healthcare organizations use to manage and exchange health information. They play a crucial role in ensuring the compatibility of their systems with HIE standards.
-
Public Health Agencies:
- Centers for Disease Control and Prevention (CDC), State Health Departments: Public health agencies leverage HIE to monitor and respond to disease outbreaks, conduct research, and gather population health data.
-
Research Institutions:
- Universities and Research Organizations: These entities may use HIE data for research purposes, contributing to advancements in medical knowledge, treatment strategies, and public health initiatives.
-
Laboratories and Diagnostic Service Providers:
- Clinical Laboratories, Radiology Centers: These providers contribute diagnostic test results and imaging reports to the HIE, enhancing the comprehensiveness of patient records.
-
Pharmacies:
- Pharmacy Chains and Independent Pharmacies: Access to a patient's medication history through HIE is valuable for pharmacists to ensure safe and effective medication management.
Collaboration among these stakeholders is essential for the success of HIE initiatives. Effective communication, adherence to standards, and a commitment to privacy and security are critical components of a successful health information exchange process.
D. Benefits and Challenges of Health Information Exchange
Benefits of Health Information Exchange (HIE):
-
Improved Patient Care:
- Access to comprehensive and up-to-date patient information enables healthcare providers to make more informed decisions, leading to improved patient care and outcomes.
-
Enhanced Care Coordination:
- HIE facilitates better coordination of care among different healthcare providers. It reduces the risk of redundant tests and procedures and ensures that healthcare teams have a complete view of a patient's medical history.
-
Efficiency and Time Savings:
- Timely access to patient information reduces the need for manual data retrieval, streamlining administrative processes, and saving time for healthcare professionals.
-
Reduced Medical Errors:
- HIE helps prevent medical errors by providing accurate and complete patient information. This includes medication reconciliation, allergy alerts, and other safety features.
-
Cost Savings:
- Avoidance of redundant tests, improved care coordination, and reduced administrative burdens contribute to cost savings for both healthcare providers and patients.
-
Public Health Surveillance:
- HIE supports public health initiatives by providing timely and accurate data for disease surveillance, outbreak monitoring, and research.
-
Patient Engagement:
- Patients benefit from increased access to their own health information, empowering them to actively participate in their care decisions and better manage their health.
-
Interoperability and Flexibility:
- HIE promotes interoperability, allowing different health information systems to work together. This fosters innovation and the integration of new technologies into healthcare delivery.
Challenges of Health Information Exchange (HIE):
-
Interoperability Challenges:
- Achieving seamless interoperability among diverse health information systems can be complex due to variations in data formats, standards, and technologies.
-
Privacy and Security Concerns:
- Protecting patient privacy and securing health information during exchange are ongoing challenges. Ensuring compliance with regulations such as HIPAA is critical.
-
Resistance to Change:
- Healthcare professionals and organizations may resist transitioning from familiar but outdated systems to new technologies, impacting the adoption and success of HIE initiatives.
-
Standardization Issues:
- Lack of uniformity in data standards and terminologies can hinder effective data exchange. Standardization efforts are crucial to address this challenge.
-
Financial Barriers:
- The initial costs of implementing HIE systems, including technology investments and training, can be a barrier, particularly for smaller healthcare organizations.
-
Legal and Regulatory Challenges:
- Navigating complex legal and regulatory landscapes, including data sharing agreements and consent management, poses challenges for HIE initiatives.
-
Data Governance and Quality:
- Ensuring the accuracy, completeness, and reliability of exchanged data is essential. Establishing robust data governance practices is critical for maintaining data quality.
-
Provider Participation and Engagement:
- The success of HIE depends on widespread participation and engagement from healthcare providers. Encouraging participation and addressing concerns are ongoing challenges.
Addressing these challenges requires collaborative efforts from stakeholders, ongoing technological advancements, and a commitment to privacy, security, and standardized data exchange in the healthcare industry. As HIE continues to evolve, overcoming these challenges will contribute to the realization of its full potential in improving patient care and healthcare delivery.
E. What are some Real-world examples of improved patient care through HIE?
Several real-world examples demonstrate the positive impact of Health Information Exchange (HIE) on patient care. These examples highlight how HIE has improved care coordination, enhanced decision-making, and contributed to better health outcomes. Here are a few noteworthy instances:
-
Reduced Emergency Department Visits:
- In Indiana, the Indiana Health Information Exchange (IHIE) implemented a system that provides emergency room physicians with access to a patient's medical history, including past diagnoses, medications, and allergies. This has led to a significant reduction in unnecessary tests and emergency department visits, as healthcare providers can make more informed decisions based on comprehensive patient information.
-
Improved Medication Reconciliation:
- In New York, the Statewide Health Information Network for New York (SHIN-NY) has implemented HIE to improve medication reconciliation. The system allows healthcare providers to access a patient's medication history, helping to avoid adverse drug interactions and ensuring that prescribed medications align with the patient's existing regimen.
-
Enhanced Care for Chronic Conditions:
- The Kansas Health Information Network (KHIN) has demonstrated success in managing chronic conditions through HIE. For patients with conditions such as diabetes or hypertension, HIE allows for a more holistic view of their health status, enabling timely interventions, medication adjustments, and improved disease management.
-
Faster and More Informed Decision-Making:
- The Utah Health Information Network (UHIN) has implemented HIE to provide real-time access to critical patient information. This has proven particularly valuable in emergency situations, allowing healthcare providers to make faster and more informed decisions, leading to improved patient outcomes.
-
Reduced Redundant Tests and Imaging:
- The Greater Houston Health Connect (GHH) in Texas has demonstrated a reduction in redundant tests and imaging procedures. With HIE, healthcare providers can access a patient's complete medical history, reducing the need for repeating tests that have already been conducted elsewhere.
-
Streamlined Referral Processes:
- In North Carolina, the North Carolina Health Information Exchange (NCHIE) has improved the referral process between primary care physicians and specialists. With HIE, specialists can access relevant patient information quickly, leading to more efficient and coordinated care.
-
Public Health Surveillance and Response:
- During the H1N1 influenza outbreak, HIE systems in various states, such as the Michigan Health Information Network (MiHIN), played a crucial role in providing timely and accurate data for public health surveillance. This facilitated a rapid response to the outbreak and helped in the allocation of resources.
These examples illustrate how HIE has positively impacted patient care by providing healthcare professionals with timely access to comprehensive patient information. This, in turn, has led to more personalized, coordinated, and efficient healthcare delivery, ultimately contributing to improved health outcomes for individuals and populations.
IV. The role of Medicai in a Health Information Exchange system
In a Health Information Exchange (HIE) system, Medicai plays a critical role in facilitating the exchange of medical images and information among different healthcare entities. Here's a breakdown of their roles:
1. Medicai's Medical Imaging Infrastructure:
-
- Storage and Retrieval: The infrastructure provides a centralized and secure repository for storing medical images. It ensures that these images are easily retrievable when needed for diagnosis, treatment planning, or consultation.
- Data Standardization: It supports standardized formats (such as DICOM - Digital Imaging and Communications in Medicine) to ensure interoperability and consistency in medical image data across different systems and healthcare providers.
- Scalability: The infrastructure must be scalable to handle the growing volume of medical images generated, ensuring that it can accommodate the needs of a diverse range of healthcare organizations.
2. Medicai's Platform:
- Collaboration and Communication: The platform facilitates collaboration among healthcare professionals by providing tools for sharing and reviewing medical images. It enables secure communication and collaboration, supporting multidisciplinary teams involved in patient care.
- Integration with Electronic Health Records (EHRs): Integration with EHR systems ensures that medical images are seamlessly incorporated into a patient's comprehensive health record. This integration enhances the overall clinical context and supports more informed decision-making.
- Workflow Optimization: Medicai helps optimize clinical workflows, allowing healthcare professionals to efficiently access, analyze, and share medical images. This contributes to improved patient care and outcomes.
3. Medicai's API (Application Programming Interface):
- Interoperability: Medicai's API enables seamless integration with other healthcare IT systems, allowing for the exchange of medical image data between different applications and platforms. This interoperability is crucial for connecting disparate systems within a health information exchange network.
- Customization and Development: Medicai's API empowers developers to create custom applications, tools, or features that leverage the capabilities of the medical imaging infrastructure and platform. This flexibility encourages innovation and the development of tailored solutions to meet specific healthcare needs.
- Secure Data Exchange: Medicai's API plays a vital role in ensuring secure and standardized data exchange between different components of the HIE system. Security protocols are implemented to protect patient information during transmission and access.
IV. What is the future of Health Information Exchange (HIE)?
The future of Health Information Exchange (HIE) holds significant promise as technology continues to advance, and healthcare systems strive to enhance interoperability, data exchange, and patient care. Several trends and developments are shaping the future landscape of HIE:
1. Enhanced Interoperability Standards:
-
- Ongoing efforts are focused on refining and expanding interoperability standards, such as Fast Healthcare Interoperability Resources (FHIR). The goal is to create a more seamless and standardized framework for sharing health information across diverse systems and platforms.
2. Population Health Management:
-
- HIE will play a crucial role in population health management initiatives. Aggregated and de-identified data from HIE can be leveraged for public health research, monitoring disease trends, and implementing targeted interventions to improve community health.
3. Artificial Intelligence (AI) and Analytics Integration:
-
- Integration of AI and advanced analytics into HIE systems will enable more robust data analysis. Predictive analytics can help identify patterns, anticipate patient needs, and support proactive healthcare interventions.
4. Telehealth Integration:
-
- The integration of telehealth and virtual care platforms with HIE will become more prevalent. This integration will support the exchange of information between remote care providers and traditional healthcare settings.
5. Standardization of Social Determinants of Health (SDOH) Data:
-
- The inclusion and standardization of Social Determinants of Health (SDOH) data in HIE will provide a more holistic view of a patient's health by considering factors such as social, economic, and environmental influences.
6. Regulatory Influence:
-
- Evolving healthcare regulations, such as those related to interoperability and information blocking, will continue to shape the direction of HIE. Compliance with these regulations will be a driving force for healthcare organizations.
7. Global Collaboration:
-
- Increased collaboration on an international scale is expected. As healthcare becomes more globalized, the ability to exchange health information seamlessly across borders will be a priority.The future of HIE lies in creating a connected, patient-centric, and data-driven healthcare ecosystem. As technology, policies, and healthcare practices evolve, HIE will continue to play a pivotal role in improving care coordination, enhancing patient outcomes, and contributing to advancements in public health.

