Federally Qualified Health Centers (FQHCs) play a pivotal role in the U.S. healthcare system by providing comprehensive primary and preventive care services to underserved and vulnerable populations.
These centers are critical in bridging the healthcare gap, particularly in rural and low-income urban areas, where access to medical care is often limited.

The Role of FQHCs
FQHCs are community-based health providers that receive funds from the Health Resources and Services Administration (HRSA) to provide primary care services in underserved areas. They must meet stringent federal requirements regarding the scope of services, quality of care, and governance. Key features of FQHCs include:
- Sliding Fee Scale Programs: These programs ensure that services are provided regardless of patients’ ability to pay. The sliding fee scale guidelines determine the discount rates based on patients’ income and family size, ensuring affordability.
- Comprehensive Care: FQHCs offer a wide range of services, including medical, dental, behavioral health, and pharmacy services.
- Patient-Centered: They emphasize patient engagement and participation in healthcare decisions, aiming to improve health outcomes and patient satisfaction.
What Makes FQHCs Different?
FQHCs are distinct from other healthcare providers due to their commitment to serving the underserved without regard to a patient’s ability to pay. They are required to operate under a sliding fee scale, which ensures that costs are adjusted based on patients’ financial capacities.
Furthermore, FQHCs are mandated to provide comprehensive services, including enabling services like transportation and language interpretation, which are often not available at other types of healthcare facilities. Their community-based and patient-centered approach fosters a healthcare environment that is both inclusive and accessible.
Impact of Community Health Centers on Underserved Populations
FQHCs have a profound impact on the health of underserved communities. They provide a safety net for millions of Americans who would otherwise lack access to essential healthcare services. For example, the Stigler Health and Wellness Center in Oklahoma serves as a crucial provider for its community, offering services on a sliding fee scale to ensure affordability for all patients.
Sliding Fee Scale Programs and Their Importance
Understanding Sliding Fee Scales
A sliding fee scale is a payment model used by FQHCs to determine the cost of services based on patients’ ability to pay. This model ensures that healthcare services are accessible to all individuals, regardless of their financial situation. The scale is calculated based on federal poverty guidelines, taking into account the patient’s income and family size.
Creating a Sliding Fee Scale
To create a sliding fee scale, FQHCs must:
- Assess Income Levels: Determine the income brackets based on federal poverty guidelines.
- Define Discount Levels: Establish discount percentages for each income bracket.
- Implement Policies: Develop policies to ensure consistent application of the sliding fee scale.
- Educate Patients: Inform patients about the availability and terms of the sliding fee program.
FQHC Revenue Cycle Management
Efficient revenue cycle management is crucial for the financial sustainability of FQHCs. This involves managing patient billing, insurance claims, and reimbursements. Key components include:
- Accurate Coding and Billing: Ensuring that all services are accurately coded and billed, including complex codes like the lung nodule CPT code.
- Timely Claims Submission: Submitting insurance claims promptly to avoid delays in reimbursement.
- Patient Follow-Up: Engaging with patients to ensure they understand their bills and any outstanding balances.
Health Innovation Technologies and FQHC EHR Systems
Adoption of Health Innovation Technologies
The adoption of health innovation technologies is essential for FQHCs to improve service delivery and patient outcomes. Technologies such as AI, telehealth, image sharing, and mobile health applications can enhance access to care, improve diagnostic accuracy, and facilitate patient engagement.
EHR Systems in FQHCs
Electronic Health Record (EHR) systems are vital for managing patient information and coordinating care. FQHCs require robust EHR systems that can handle the unique needs of their patient populations. Features to look for in FQHC EHR software include:
- Comprehensive Patient Records: Maintaining detailed and accurate patient records.
- Interoperability: Ensuring seamless data exchange with other healthcare providers and systems.
- Patient Engagement Tools: Providing tools for patients to access their health information and communicate with their healthcare team.
Challenges Faced by FQHCs
FQHCs face several challenges in delivering quality healthcare services, including:
- Funding Constraints: Limited funding can restrict the scope and quality of services offered.
- Workforce Shortages: There is often a shortage of healthcare providers willing to work in underserved areas.
- Patient Volume: High patient volume and large patient panel sizes by specialty can strain resources and affect the quality of care. For instance, the average number of patients seen per day by a physician assistant in an FQHC setting can be quite high.
The Role of Medical Imaging Access in FQHCs
Importance of Medical Imaging
FQHCs integrate medical imaging services into their care models to enhance diagnostic capabilities and improve patient outcomes. The inclusion of imaging technologies, such as X-rays, ultrasounds, and MRIs, allows for early detection and better management of diseases.
Cancer Screening at FQHCs
Cancer screening is a critical preventive service provided by FQHCs. Early detection through screenings such as mammograms, Pap smears, and colonoscopies significantly improves the chances of successful treatment and survival. FQHCs often focus on cancers with high prevalence rates, such as breast, cervical, and colorectal cancer.
Addressing Cancer in High-Risk States
Certain U.S. states, such as Kentucky, West Virginia, and Mississippi, have the highest rates of cancer. FQHCs in these states play a crucial role in offering accessible cancer screening services to populations at elevated risk. By targeting high-risk groups, FQHCs help reduce cancer incidence and mortality rates.
Oatmeal Health and Its Role in Cancer Screening
Oatmeal Health is a company dedicated to enhancing health equality through AI-enabled cancer screening and early detection. The platform focuses on underserved FQHC patient populations, offering expert primary care support, comprehensive radiology risk assessments, and cutting-edge AI. Oatmeal Health provides these services at no cost, fully funded by Medicare and Medicaid.
Oatmeal Health leverages advanced AI technologies to improve the accuracy and efficiency of cancer screenings. The AI algorithms assist in interpreting medical images, identifying potential abnormalities, and prioritizing cases that require further investigation. This technological innovation is crucial in areas with limited access to specialized radiologists.
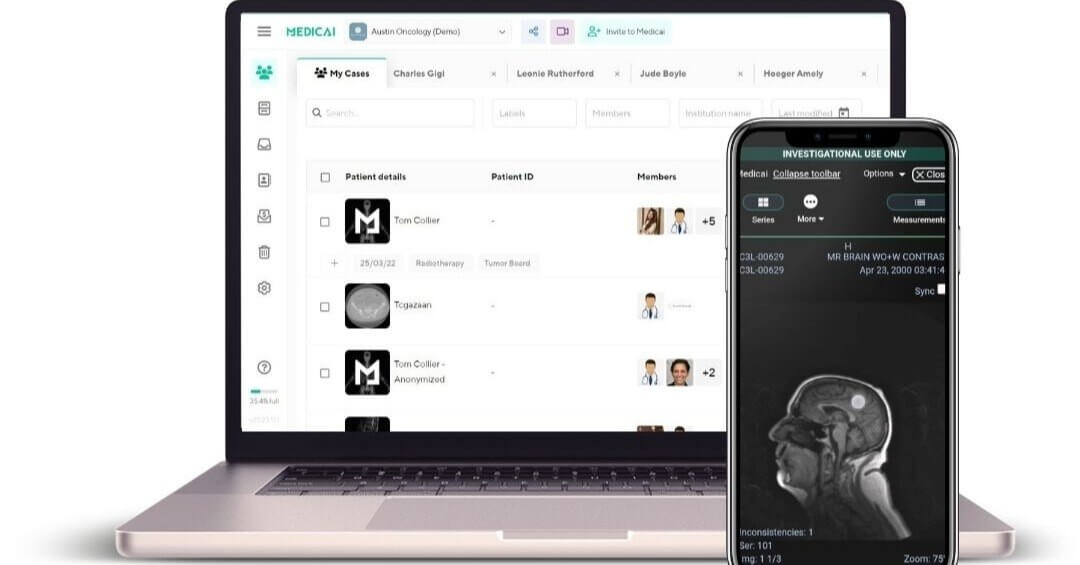
How can Medicai Support FQHCs?
Enhancing Imaging Capabilities
Medicai offers solutions that can significantly enhance the imaging capabilities of FQHCs. The platform provides seamless integration of medical imaging services, enabling FQHCs to efficiently communicate with imaging centers.
Streamlining Workflows and Patient Management
Medicai’s solutions also streamline workflows and improve patient management at FQHCs. The platform facilitates image sharing and collaboration among healthcare providers. This ensures that patients receive timely and accurate diagnoses, leading to better health outcomes.

Conclusion
FQHCs are indispensable in providing healthcare to underserved populations, offering comprehensive services on a sliding fee scale to ensure affordability. Medical imaging and cancer screening are crucial components of their service offerings, enabling early detection and improved outcomes for conditions like cancer.
By integrating cutting-edge technologies and providing no-cost services funded by Medicare and Medicaid, Oatmeal Health significantly contributes to health equality.
Medicai’s support in enhancing imaging capabilities and streamlining workflows further empowers FQHCs to deliver high-quality care.
Through continued innovation and dedication to patient-centered care, FQHCs, along with partners like Oatmeal Health and Medicai, can continue to advance health equity and improve outcomes for underserved populations across the United States.
Enhance FQHC Care with Medicai’s Image Sharing Services
Federally Qualified Health Centers (FQHCs) are the backbone of healthcare for underserved communities, ensuring access to comprehensive and quality care. As the healthcare landscape evolves, it’s crucial for FQHCs to adopt innovative solutions that enhance care coordination, improve patient engagement, and reduce costs. Medicai’s image sharing services offer a transformative solution to these challenges.
Why Adopt Medicai’s Image Sharing Services?
- Improved Care Coordination:
- Seamless Integration: Medicai’s platform integrates effortlessly with existing Electronic Health Record (EHR) systems, allowing for smooth exchange of imaging data.
- Collaborative Care: Facilitate real-time collaboration between primary care providers, specialists, and radiologists, ensuring that every team member has immediate access to the most up-to-date imaging results.
- Enhanced Patient Engagement:
- Patient Access: Empower patients by providing them with easy access to their medical images and reports through a secure, user-friendly portal.
- Better Communication: Improve patient understanding and involvement in their care by enabling them to share images with other healthcare providers, ensuring continuity and comprehensiveness of care.
- Cost Reduction:
- Efficiency Gains: Reduce administrative overhead and duplication of imaging studies by centralizing image storage and sharing.
- Resource Optimization: Free up valuable time and resources by minimizing the need for physical transfer of imaging data, leading to faster diagnosis and treatment.
FAQs
What are the problems facing FQHC?
Federally Qualified Health Centers (FQHCs) are critical components of the U.S. healthcare system, providing essential services to underserved populations. Despite their importance, FQHCs face numerous challenges that impact their ability to deliver high-quality patient care.
Funding Challenges
One of the primary issues facing FQHCs is funding. Although they receive federal funding, this financial support is often insufficient to cover all operational costs. The reliance on Medicaid reimbursement and Medicare funding further complicates financial stability, as reimbursement rates can be low and unpredictable. This funding shortfall can limit the scope of services provided and affect the overall sustainability of these centers.
Staffing Challenges
FQHCs frequently encounter staffing challenges. Recruiting and retaining qualified healthcare professionals, such as doctors and clinicians, is particularly difficult in underserved and rural areas. Clinicians and other staff members often face heavy workloads due to high patient volumes, leading to burnout and high turnover rates. These staffing issues can compromise the quality of clinical services and patient care.
Access to Healthcare and Health Disparities
Ensuring access to healthcare for all patients, including uninsured patients and Medicaid beneficiaries, remains a significant challenge. Health disparities are prevalent in the communities served by FQHCs, often stemming from socioeconomic factors, geographic barriers, and limited healthcare resources. These disparities can result in poorer health outcomes and increased strain on FQHCs to meet the needs of their patient populations.
Integration of Health Systems and Technologies
The integration of health systems and the adoption of new technologies, such as telehealth services and remote patient monitoring, present both opportunities and challenges. While these technologies can enhance the patient experience and expand access to care, implementing and maintaining them can be resource-intensive. FQHCs may struggle with the initial costs and ongoing management of these technologies, impacting their ability to fully leverage the benefits.
Coordination with Other Healthcare Organizations
FQHCs must often coordinate care with other healthcare organizations, including hospitals and clinics. Effective coordination is essential for providing comprehensive care, but it can be challenging due to differences in systems, policies, and resource availability. This lack of seamless coordination can hinder the continuity of care for patients.
Patient Volume and Care Quality
High patient volume is a common issue for FQHCs, which can affect the quality of care provided. With limited staff and resources, FQHCs may struggle to manage the large number of patients seeking care. This high demand can lead to longer wait times, shorter consultation periods, and potential compromises in the quality of patient care.
Mission-Driven but Resource-Constrained
FQHCs operate with a mission to provide accessible, high-quality healthcare to all individuals, regardless of their ability to pay. However, this mission-driven approach often comes with resource constraints. Balancing the commitment to community health and the realities of limited financial and human resources is a constant challenge for these health centers.
Medicaid and Medicare Reimbursement
The financial health of FQHCs is closely tied to Medicaid and Medicare reimbursement. Variations in state Medicaid programs and reimbursement rates can create financial uncertainty. Additionally, the complex process of billing and reimbursement can strain administrative resources, diverting attention from direct patient care.
FQHCs are vital in addressing healthcare needs in underserved communities, but they face a myriad of challenges. From funding and staffing issues to the integration of new technologies and coordination with other healthcare organizations, these challenges require strategic solutions and support from both federal and state levels. By addressing these problems, FQHCs can continue to fulfill their mission of providing high-quality, accessible care to the nation’s most vulnerable populations.




