Why images still fail to open across systems — and how modern cloud PACS like Medicai solve the DICOM interoperability failures.
Healthcare assumes medical imaging should be universally compatible, aka interoperability. A CT scan produced in one hospital should load seamlessly on a workstation in another. An MRI from a Siemens machine should display correctly on a GE viewer. A patient study should follow the radiologist across PACS, portals, and cloud systems without losing fidelity or metadata.
But real-world radiology tells a different story. DICOM interoperability — in theory a solved problem — remains one of the biggest operational headaches in medical imaging. Hospitals still encounter unreadable studies, lost series, failed sends, incompatible transfer syntaxes, and PACS migrations that corrupt years’ worth of imaging records.
This article breaks down why DICOM interoperability breaks, how hospitals diagnose the failure, and why cloud-native platforms like Medicai now offer the most reliable path forward.

DICOM Interoperability Failures: The Problems No One Talks About
Despite being a global imaging standard, DICOM is interpreted differently by each vendor. The standard is stable; implementations are not. This mismatch is the root cause of most interoperability failures.
1. AE Title, Port, and IP Mismatches: The Classic “Send Failure”
For a DICOM file to transfer successfully between systems, three values must align perfectly: the AE Title, the port number, and the device’s IP address. If any of these differ — even by one character — the receiving system silently rejects the incoming study. Radiology teams often spend hours chasing down these silent failures, usually armed only with vague logs.
A modern platform like Medicai avoids this guessing game. It provides real-time status logs, connection indicators, and detailed error messages so teams can pinpoint misconfigurations instantly.
2. Transfer Syntax Incompatibility: When the Image Arrives but Won’t Display
Many older PACS systems simply cannot decode modern compression methods such as JPEG-LS or JPEG2000 Lossless. The result is an image that technically “arrives,” but shows nothing but a blank screen. This is especially common with enhanced MRI, cardiac CT, and high-resolution studies.
Medicai’s pipeline supports virtually all transfer syntaxes, ensuring pixel data renders correctly regardless of which scanner produced it.
3. SOP Class Mismatches: Enhanced Objects That Older Systems Can’t Read
Each DICOM file carries a SOP Class UID that identifies what kind of object it is — a CT slice, an ultrasound cine loop, a PET volume, a segmentation object, and so on. Legacy PACS were never designed for modern enhanced MR objects, DICOM-SEG files, or radiotherapy objects. As a result, studies arrive incomplete, missing key series, or fail entirely.
Medicai was built to ingest enhanced and structured objects natively, which is essential for oncology, radiotherapy, and AI-driven imaging workflows.
4. Corrupted or Incomplete Metadata: When the “Glue” Breaks
Metadata gives meaning to the pixel data. If the Study Instance UID is duplicated, if character sets are invalid, or if key tags are missing, the PACS cannot properly group images into a coherent study. This causes series to fragment, images to appear as unrelated files, or studies to scatter across the archive.
Medicai automatically repairs metadata, reconstructs missing fields, and normalizes inconsistent tags, transforming unusable studies into clinically readable datasets.
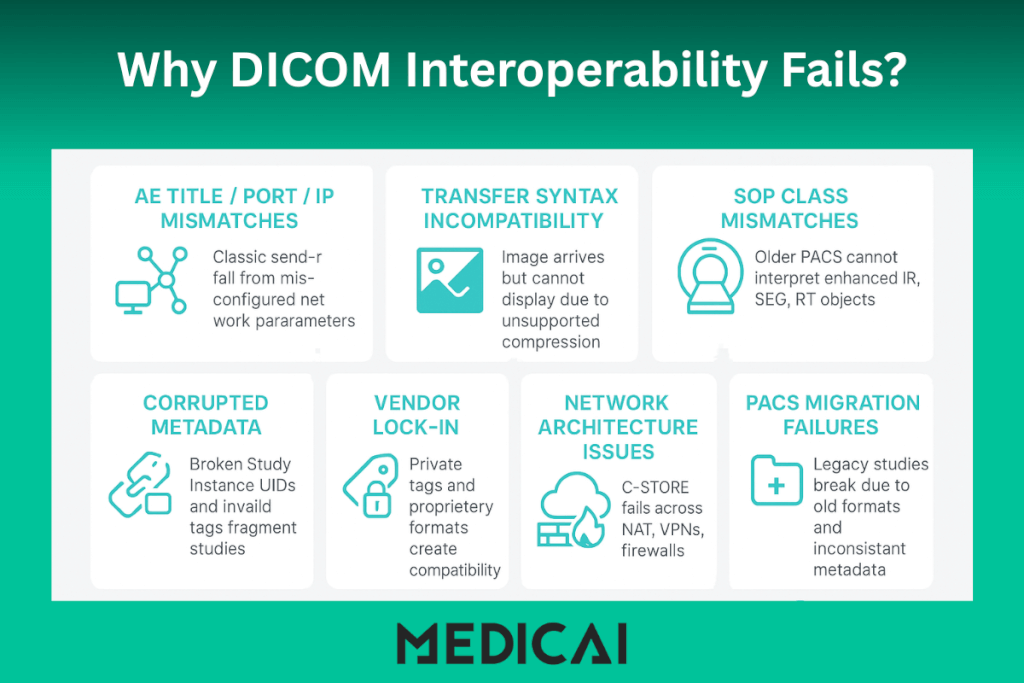
5. Vendor Lock-In and Proprietary Implementations
Before the cloud era, vendors routinely inserted private tags, custom compression methods, and proprietary metadata structures into their imaging systems. These technically follow the DICOM standard, but cause incompatibilities when opened on other systems.
Medicai resolves this by translating proprietary elements, stripping unnecessary ones, and mapping private tags to standard fields whenever possible.
6. Network Architecture Issues: DICOM Was Not Designed for Firewalls or NAT
Traditional DICOM C-STORE communication requires two devices to “see” each other on a network. In today’s world of VPNs, NAT, segmented networks, and cloud endpoints, this becomes fragile. Even minor network changes can disrupt hundreds of imaging transfers.
Medicai bypasses these constraints entirely by relying on DICOMweb — a modern HTTP-based protocol that works reliably over today’s network infrastructure.
7. PACS Migration Failures: The Silent Killer of Interoperability
Hospitals switching from one PACS to another often discover that thousands of older studies no longer open correctly. Enhanced CT objects may fail to render, private tags may conflict, and legacy compression formats may break modern viewers.
Medicai uses normalization, transcoding, and metadata repair to ensure that even the oldest studies remain fully viewable.
How Radiology Teams Diagnose DICOM Interoperability Problems
Most hospitals still rely on trial-and-error. IT teams inspect PACS logs line by line, re-send studies repeatedly, or test connections manually. Logs often display cryptic messages such as “Association rejected” or “No presentation context accepted,” leaving radiologists frustrated and patients waiting.
Cloud-native platforms make diagnosis far simpler. Radiology teams can view ingestion logs in real time, receive automated error classifications, and inspect metadata directly in the viewer. This reduces hours of troubleshooting to minutes.
Why Legacy PACS Struggle — And Why Cloud PACS Fix the Problem
Legacy PACS were built in an era when imaging workflows stayed inside one hospital, when scanners were few, and when networks were closed systems. Today’s workflows are distributed, multi-hospital, AI-powered, and cloud-dependent. Old PACS were never designed for modern interoperability.
Cloud PACS fundamentally changes the model. Since storage, decoding, normalization, and routing all occur in the cloud, compatibility issues can be resolved at the platform level rather than at the hardware level.
How Medicai Solves DICOM Interoperability Automatically
Medicai provides a modern ingestion engine that handles the complexity that legacy systems couldn’t anticipate.
The platform receives imaging through DICOMweb, gateway applications, and drag-and-drop uploads — eliminating traditional network configuration hurdles. Once images arrive, Medicai performs on-the-fly metadata repair, UID normalization, and transfer syntax conversion. Instead of failing, studies adapt to the viewer.
Medicai also supports enhanced DICOM objects, segmentation files, radiotherapy data, and multi-frame imaging, making it suitable for oncology and advanced diagnostic workflows. The system automatically groups series accurately, recognizes duplicates, and reconstructs multi-frame volumes. The result is a clean, corrected, fully readable study — even when the originating equipment is decades old.
Sharing becomes effortless as well. Instead of burning CDs or sending unencrypted emails, clinicians generate secure viewer links that work on any device, anywhere, without software installation.
Real Case Example: When a CT Upgrade Broke a Clinic’s PACS
A cancer clinic upgraded one of its CT scanners, which began producing enhanced CT objects and JPEG2000 images. Their old PACS could ingest the files, but could not display them. Radiologists saw blank images, and tumor board cases backed up for days.
After switching ingestion to Medicai, all transfer syntaxes were decoded properly, metadata was repaired automatically, and enhanced objects were rendered without errors. What had caused days of disruption in their legacy PACS became a non-event in the cloud.
The Future of Interoperability: DICOM Without Friction
With cloud-native PACS, DICOMweb, AI-driven tag repair, and universal web viewers, interoperability will finally become a guaranteed outcome instead of a gamble. Medicai is part of the next wave of imaging infrastructure designed for cross-hospital data continuity, radiologist mobility, and seamless AI integration.
The future belongs to systems that treat DICOM interoperability not as a technical challenge but as a solved problem — and Medicai is helping define that standard.


