If you walk into the reading room of a typical private radiology practice or a large hospital network today, you will see a chaotic scene.
You will see a radiologist sitting at four monitors, using three keyboards, logging into five PACS systems. They are frantically “Alt-Tabbing” between windows, trying to remember if the acute stroke patient is in the “Memorial Hospital” queue (System A) or the “Community Clinic” queue (System B).
This is the “Swivel-Chair” Workflow.
It is the single biggest driver of radiologist burnout, administrative inefficiency, and blown Turnaround Times (TAT). In an era of consolidation, where groups are servicing more sites than ever, the friction of logging into multiple disparate systems is unsustainable.
The traditional IT answer has been terrifying: “We need to rip everything out and migrate everyone to one giant monolithic PACS.” That costs millions of dollars and takes years.
But there is a better way. This guide explores the Unified Worklist strategy—an “Overlay Architecture” that allows you to connect disparate PACS systems without replacing them, creating a single, harmonious reading environment.

The Fragmentation Crisis: How We Got Here
Fragmentation is rarely a choice; it is a consequence of growth.
Most healthcare networks today are the result of Mergers and Acquisitions (M&A).
- Scenario A: A large IDN (Integrated Delivery Network) buys three smaller community hospitals. The main hospital uses Sectra, but the new acquisitions use GE and Fujifilm.
- Scenario B: A private radiology group wins a contract to read for a new urgent care chain that refuses to switch its PACS.
The result is a “Frankenstein” network. The data is trapped in silos. The patient who had a CT scan at the urgent care (System A) and then went to the ER (System B) has a split medical record. The radiologist reading the ER scan often doesn’t know the prior CT exists because they are looking at a different worklist.
The Hidden Cost of “Swivel-Chair” Interoperability
While the technical problem is “fragmentation,” the business problem is waste. The “Swivel-Chair” workflow bleeds money and morale in three specific ways:
A. The Productivity Tax
Every time a radiologist has to log out of one system and log into another, they lose focus. Cognitive science tells us that “context switching” carries a heavy penalty. If a doctor spends 30 minutes a day just navigating login screens and managing disparate queues, that is 30 minutes of lost billable reading time. Across a group of 20 radiologists, that is thousands of exams per year left unread.
B. The “Cherry-Picking” Problem
When worklists are fragmented, orchestration becomes impossible. Radiologists naturally gravitate toward the “easy” queue or the system with the best interface. Complex cases hidden in a clunky, secondary PACS queue often sit unread until the TAT is blown, leading to angry referring physicians and potential SLA penalties.
C. The Clinical Risk (Missing Priors)
This is the most dangerous consequence. If a radiologist is reading a Chest X-Ray in System A, but the patient’s prior Lung CT is locked in System B, the doctor is flying blind. They might recommend an unnecessary biopsy for a nodule that has been stable for five years—simply because they couldn’t see the history.
Why “Rip and Replace” Is Not the Answer
When faced with fragmentation, the knee-jerk reaction from traditional PACS vendors is to consolidate. “Just migrate all your data to our Big Iron system.”
This is a trap for three reasons:
- Cost: Migrating 10 years of data from five different hospitals is an expensive, six-figure project.
- Politics: The smaller hospitals you acquired might love their current PACS. Forcing them to switch causes staff revolt and training nightmares.
- Downtime: Data migrations are risky. Records get corrupted, links break, and systems go down.
You do not need to replace the underlying storage to fix the workflow. You need an Integration Layer.
The Solution: The “Overlay” Architecture
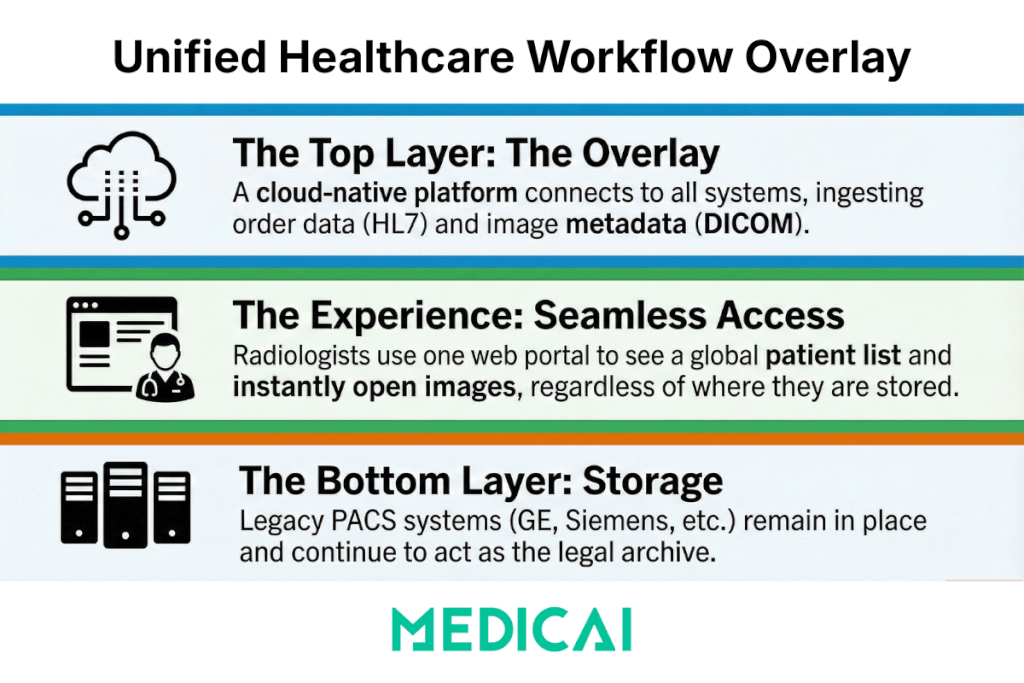
The modern solution is to implement a Unified Worklist (often powered by a VNA or Workflow Orchestrator).
Think of this as a “Manager” layer that sits on top of your disparate PACS systems.
- Bottom Layer (Storage): The legacy PACS (GE, Siemens, etc.) stay exactly where they are. They continue to act as the legal archive for their respective sites.
- Top Layer (The Overlay): A cloud-native platform (like Medicai) connects to all of them. It ingests the order data (HL7) and the image metadata (DICOM).
- The Experience: The radiologist logs into one web portal. They see one global list: “Patient Smith (Hospital A)” next to “Patient Jones (Clinic B).”
When they click “Open,” the Overlay system pulls the images from the correct source instantly. The doctor never knows—and never cares—where the data actually lives.
Under the Hood: The Tech Stack of Unification
How does this work technically? It relies on three critical integration engines: HL7 Normalization, DICOM Routing, and the MPI.
A. The Universal Translator (HL7 & FHIR)
Hospital A calls a “CT Head” procedure code CT-HEAD-WO. Hospital B calls it 70450. If you put these on one list, it looks like a mess. A robust Unified Worklist uses a Normalization Engine. It maps these disparate codes to a standard “Global Procedure Code.” It ensures that “Stat,” “Urgent,” and “ASAP” all map to the same high-priority red flag in the viewer.
B. The Master Patient Index (MPI)
This is the brain of the operation.
- In System A, the patient is “Jonathan Smith, DOB 01/01/80.”
- In System B, he is “Jon Smith, DOB 01/01/1980.” A dumb system sees two people. An MPI-enabled system uses probabilistic matching (fuzzy logic) to realize this is the same person. It automatically links the records.
- The Result: When the radiologist opens the case, the system presents the current exam alongside the prior exams from the other facility automatically.
C. Smart DICOM Routing (Prefetching)
You don’t want to download the entire archive to the cloud. You only need the relevant data. The Overlay system uses Smart Prefetching logic. When an order comes in via HL7 ORM:
- The system queries all connected nodes: “Does anyone have priors for this patient?”
- It routes the new images and the relevant priors to the cloud cache.
- It serves them via Server-Side Rendering to the radiologist’s browser.
The Clinical & Operational Impact
Implementing a Unified Worklist transforms the economics of a radiology practice.
- Load Balancing: You can now implement “Global Reading.” If the radiologist at Hospital A is swamped, but the radiologist at Hospital B is quiet, the system can route Hospital A’s cases to Hospital B’s worklist instantly. You maximize the utilization of your workforce.
- Reduced Burnout: Radiologists get their lives back. One login. One interface. No more password fatigue. A happier radiologist is a faster, more accurate radiologist.
- Improved TAT: By eliminating the “toggle tax” and enabling automated worklist prioritization (e.g., “Show all Stroke cases at the top”), groups often see a 20–30% reduction in Turnaround Time.
Strategic Advantage: Medicai as the Glue
This is where Medicai fits into your strategy.
We are not just another PACS vendor trying to force you into a proprietary box. We are the Integration Layer. Medicai is built on an API-first, Cloud-Native VNA architecture explicitly designed for this “Overlay” use case.
- Connect Anything: Our Gateway technology can ingest data from any legacy PACS (DICOM) or EMR (HL7/FHIR) without requiring complex VPNs.
- Zero-Footprint Viewer: Your radiologists can read from anywhere—hospital, home, or hotel—using a diagnostic-grade web viewer that handles the heavy lifting in the cloud.
- Vendor Agnostic: We don’t care if you use Sectra, Philips, or a dusty old server in a closet. We unify them all.
Conclusion: Unity Without Destruction
The future of radiology is not “One Giant Server.” The future is Interoperability.
You do not need to destroy your existing infrastructure to fix your workflow problems. By adopting a Unified Worklist strategy, you can respect the autonomy of your individual sites while giving your radiologists a single, powerful tool to do their jobs.
Stop the swivel-chair madness. Start reading as one team.




