Cancer imaging is evolving fast, and so are the expectations. Clinicians need instant clarity, patients deserve precision, and radiologists face growing pressure to deliver both.
Structured annotations in oncologic reporting embed standardized data onto PACS images, creating faster, clearer reports and streamlining radiology workflows. This innovation enhances clinical communication, supports tumor tracking, and produces research-quality datasets in routine practice.
Let’s discover how structured annotations work, the benefits they bring, and why they’re set to redefine oncologic reporting for the future.

The Problem with Conventional Oncologic Reporting
Modern cancer care demands quick and precise imaging reports, but many radiologists rely on outdated methods, causing delays and variations. This slows decision-making, increases communication with clinicians, and leads to missed opportunities for better patient care.
Below are some of the biggest challenges with today’s oncologic reporting workflows.
Variability in Free-Text Reports
In cancer imaging workflows, free-text reports are common, allowing radiologists to detail findings. However, this leads to variability in presentation, as two radiologists may report the same scan using different terms and structures.
Such inconsistency can confuse oncologists, delay decisions, and risk misinterpretation when determining treatment plans.
Difficulties in Tracking Tumors Over Time
Tracking a patient’s disease over time presents a challenge due to inconsistent formats, making it difficult to compare current and past scans. Oncologists often have to navigate lengthy narratives to determine if a tumor has changed. This lack of standardization can delay care, especially in multi-organ cancers.
Uneven Adoption of Structured Reporting
Even structured reporting, which was designed to solve these issues, hasn’t reached universal use. According to a survey, only about 57% of radiologists use structured reporting daily.
That means nearly half still rely on free text, leaving significant room for inconsistency and missed opportunities for efficiency.
Time-Consuming Manual Work
Manual dictation and annotation also take time. Radiologists often spend precious minutes describing lesion sizes, locations, and staging details. Sometimes they repeat the same types of measurements for different cases.
Without automation, this repetitive work can add to workload pressure, which is already a growing concern in oncology imaging.
From Structured Reporting to Structured Annotations: What’s the Difference?
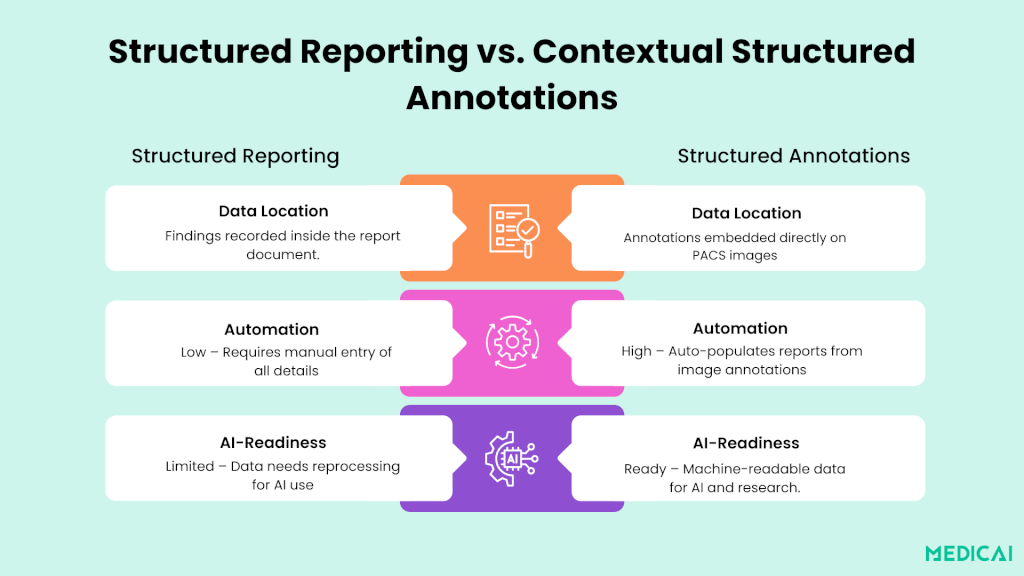
Structured reporting (SR) was a significant advancement for radiology, particularly in oncology. It introduced templates, standardized language, and a logical flow for imaging reports.
But while SR improves clarity and consistency, it still has its limits, particularly when it comes to speed, automation, and data usability for research and AI.
This is where contextual structured annotations come in. They take the principles of SR and embed them directly into the PACS workflow, making the process faster, smarter, and more connected to modern healthcare needs.
What Structured Reporting Brings to the Table
Structured reporting organizes reports into sections like “Findings” and “Impression,” often with pre-set fields for tumor size, location, and stage. It ensures completeness and makes it easier to compare exams.
Most SR users see better report quality, fewer errors, and improved communication with clinicians. However, SR still relies heavily on manual entry, as the radiologist must type or dictate every detail into the template.
What Structured Annotations Add
Structured annotations go beyond filling in a report. They allow radiologists to place machine-readable tags directly onto the image in PACS.
Each annotation can include precise lesion details, such as type, measurement, TNM stage, and even level of suspicion. This information is automatically pulled into the final report without retyping.
Embedding annotations directly in images reduces transcription errors and ensures consistent reporting. Using standardized data to track lesions over time allows for machine-readable annotations in AI and cancer research, eliminating manual labeling.
How Contextual Structured Annotations Work in PACS
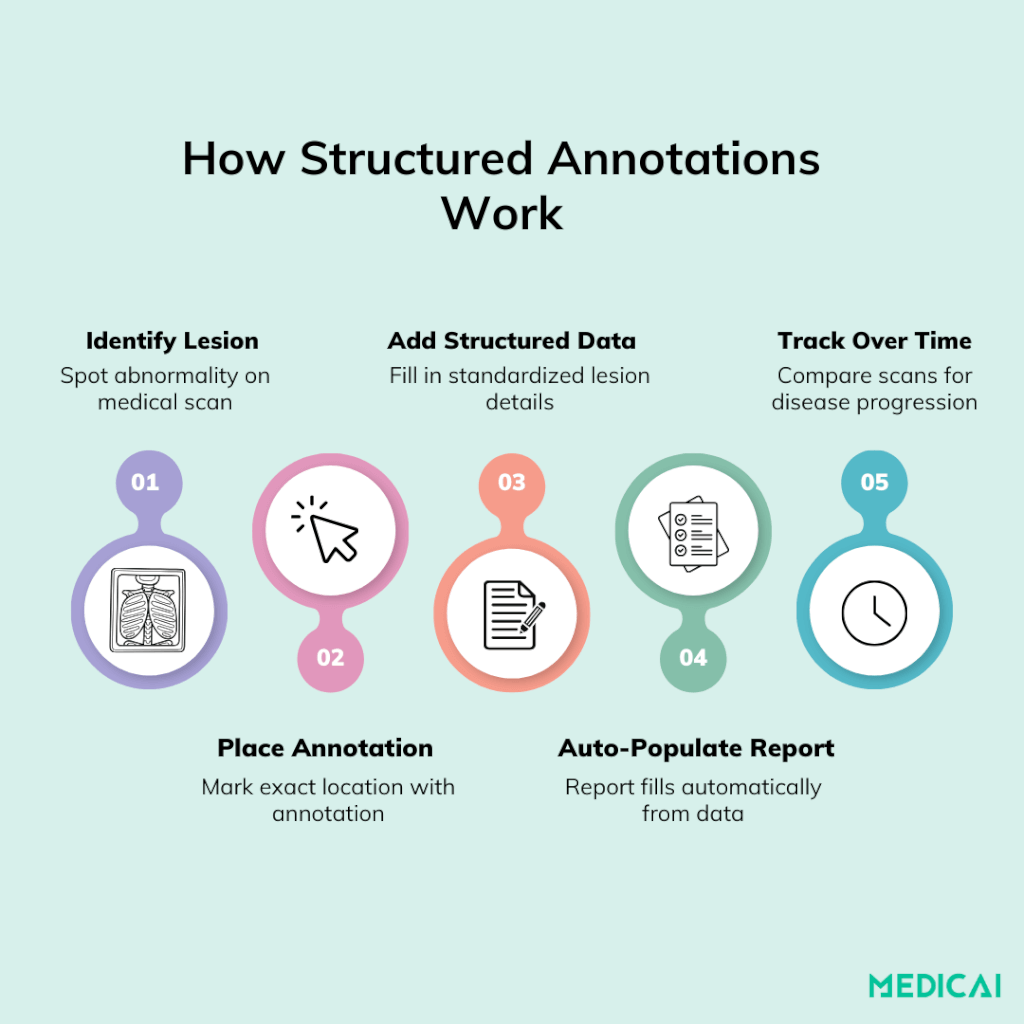
Contextual structured annotations enhance radiologists’ workflows by enabling direct data capture on PACS images, speeding up the process and reducing errors.
Step 1: Identify the Lesion
The workflow starts like any other. The radiologist reviews the scan and spots an abnormality. But instead of mentally noting details to dictate later, they take action immediately.
Step 2: Place the Annotation
Using either a simple click on the image or a voice command, the radiologist creates an annotation tied to the exact location of the finding. This is not just a label, it’s a data point.
Step 3: Add Structured Data
Each annotation can store multiple pieces of information:
- Lesion type (e.g., primary tumor, metastasis)
- Measurements (uni- or bidimensional)
- TNM stage or treatment response category
- Diagnostic confidence level
This data is encoded in a machine-readable format, making it accessible for both human readers and AI systems.
Step 4: Auto-Populate the Report
The PACS automatically integrates these annotations into the structured report template. Instead of dictating measurements or staging, the radiologist simply confirms the details are correct. The rest is done by the system.
Step 5: Enable Longitudinal Tracking
Because annotations are linked to exact image coordinates and stored in a structured way, it’s easy to track the same lesion across multiple scans. This supports more precise monitoring of treatment response and early detection of disease progression.
Clinical Advantages of Structured Annotations
Contextual structured annotations bring clear, measurable benefits to oncology imaging workflows.
Greater Clarity for Multidisciplinary Teams
Free-text reports often require interpretation, which can lead to back-and-forth communication. Structured reporting reduces follow-up calls and emails from clinicians in nearly 79% of cases.
With structured annotations, every finding is clearly labeled, precisely measured, and tied to its exact image location. This leaves less room for misunderstanding during tumor boards or treatment planning meetings.
Faster and More Accurate Reporting
Structured annotations auto-populate the report with lesion details as soon as they’re marked in PACS. This cuts down manual dictation time and reduces the chance of transcription errors.
By standardizing lesion descriptors and measurements, radiologists can produce high-quality reports without sacrificing speed.
Improved Longitudinal Tumor Tracking
Because each annotation is linked to a specific image coordinate, tracking a lesion over time becomes much easier. Radiologists and oncologists can instantly compare changes in size, shape, or staging, helping them detect treatment responses or early signs of progression.
Support for Cancer-Specific Reporting
The survey showed strong support for including tumor stage and treatment response in reports. Structured annotations make this seamless by embedding those details directly at the point of annotation.
Whether it’s TNM staging or a RECIST-based response category, the information is structured and ready for both clinical care and research use.
Research, AI, and the Future Vision
Contextual structured annotations revolutionize oncologic reporting by enabling routine imaging studies to contribute to research, AI development, and precision cancer care.
Routine Annotations as Built-In Datasets
PACS annotations provide valuable, machine-readable information like lesion type, location, and diagnostic confidence. It transforms daily reporting into a continuous data-generation process.
The process balances the need for separate manual labeling for AI training, as data is seamlessly collected during routine clinical work.
Boosting AI Performance Through Standardization
AI algorithms require consistent, high-quality input. Structured annotations standardize lesion descriptions and measurements, reducing variability in free-text reports.
The uniformity enhances the accuracy of AI models in detecting abnormalities, segmenting tumors, and predicting treatment outcomes.
Unlocking Multi-Center and Big-Data Research
Structured annotations use standardized terminology and formats, facilitating data sharing and comparison between institutions. The approach supports large-scale radiomics studies, multi-center clinical trials, and big-data oncology research, accelerating discoveries and enhancing the generalizability of findings.
The Future: AI-Enhanced Annotation Workflows
Looking ahead, the combination of AI and structured annotations could make workflows even more efficient. AI tools will be able to pre-identify suspicious lesions, suggest annotations, and pre-fill staging details.
Radiologists can then review, confirm, or adjust these suggestions, creating a feedback loop that continuously improves both human efficiency and AI accuracy.
A Fully Integrated Oncology Imaging Ecosystem
The ultimate vision is a seamless environment where imaging, reporting, AI analysis, and longitudinal tracking are all connected.
- Tumor boards could access annotated images with instant visual summaries of disease progression.
- Treatment teams could receive automated, standardized updates on tumor changes.
- Researchers could tap into massive, clean datasets without disrupting clinical workflows.
In this ecosystem, every scan would not only guide today’s care but also contribute to improving cancer diagnosis and treatment for the future.
Overcoming Adoption Barriers
Adopting contextual structured annotations in oncologic imaging is both a technical and cultural shift. Success depends on addressing real-world challenges from workflow disruption to resource limitations.
Ensuring Technical Compatibility
Structured annotation tools must integrate smoothly with existing PACS and reporting systems, using standards like DICOM SR and HL7 FHIR. Medicai is built for this kind of interoperability, ensuring annotations flow into reports without costly infrastructure changes.
Minimizing Workflow Disruption
Radiologists need tools that fit naturally into their existing routines. One-click annotation placement, intuitive interfaces, and voice-enabled data entry can speed adoption while avoiding extra steps.
Training and Change Management
Clear onboarding and pilot programs help ease the learning curve. Role-based training, internal champions, and ongoing support can accelerate adaptation and ensure consistent use.
Managing Costs
Smaller or phased rollouts help manage budgets while proving value in high-impact areas like oncology. Medicai supports incremental deployments, allowing institutions to expand as benefits become clear.
Conclusion
Contextual structured annotations enhance communication, streamline workflows, and prepare oncology data for AI. By embedding standardized details into PACS images, radiologists can improve reporting and collaboration, and create research-ready datasets efficiently.
Medicai makes this future achievable through seamless PACS integration, intuitive annotation tools, and compliance with industry standards. We help institutions adopt smarter cancer care now, paving the way for future innovation.




