What are the differences between an MRI and an MRA? These imaging tests sound similar and use the same machine, but they aren’t interchangeable.
An MRI captures detailed images of organs and tissues, while an MRA focuses specifically on blood vessels and blood flow. They serve different diagnostic purposes, even though they rely on the same core technology.
This blog will break down the key differences between MRI and MRA in clear, simple terms so you know exactly what to expect and why it matters.

Difference Between MRI and MRA
MRI (Magnetic Resonance Imaging) and MRA (Magnetic Resonance Angiography) are non-invasive imaging techniques that use magnetic fields and radio waves. MRI examines soft tissues and organs, while MRA focuses on visualizing blood vessels to assess cardiovascular conditions.
What Is an MRI?
MRI, or Magnetic Resonance Imaging, is a non-invasive scan that uses strong magnets and radio waves to create detailed images of the inside of your body. It works by detecting signals from hydrogen atoms in your body’s water and converting them into clear images of organs, tissues, and bones.
MRI is commonly used to examine:
- The brain and spinal cord
- Joints and soft tissues like muscles and ligaments
- Internal organs such as the liver, heart, and kidneys
- Some blood vessels, though, for detailed vascular imaging, an MRA is preferred
Doctors use MRI technology to identify various medical conditions, including brain tumors, strokes, and multiple sclerosis. It also helps diagnose spinal cord issues, disc problems, joint injuries, and soft tissue damage, as well as organ diseases and some types of cancer.
Because MRI doesn’t use radiation, it’s often considered a safer option, especially for children, pregnant patients, or those needing repeated scans.

What Is an MRA?
MRA, or Magnetic Resonance Angiography, is a type of MRI that focuses specifically on blood vessels. It uses the same machine as a standard MRI but applies specialized techniques to capture images of blood flow through arteries and veins.
MRA is designed to visualize:
- Arteries and veins in the neck, brain, heart, legs, and kidneys
- The structure and function of blood vessels, often with the help of contrast dye for clearer detail
Magnetic resonance angiography (MRA) is used to detect vascular conditions, including aneurysms, narrowed arteries, blood clots related to strokes, and vascular malformations. It usually provides insight into overall vascular health.
MRA is often preferred over traditional angiograms because it provides a clear view of the circulatory system without the use of radiation, especially when non-invasive imaging is necessary.
MRI vs. MRA: The Key Differences
Although both MRI and MRA use the same technology—magnetic fields and radio waves—their purposes, techniques, and diagnostic roles differ significantly.
| Feature | MRI (Magnetic Resonance Imaging) | MRA (Magnetic Resonance Angiography) |
| Primary Focus | Organs, tissues, bones, joints | Blood vessels and blood flow |
| Examines | Brain, spine, muscles, organs, joints | Arteries and veins in brain, neck, heart, limbs |
| Contrast Use | Sometimes needed | Often required for clearer vessel images |
| Imaging Detail | Soft tissue and structural anatomy | Vascular anatomy and blood flow |
| Common Uses | Tumors, joint injuries, MS, organ disease | Aneurysms, clots, blockages, vascular malformations |
| Technique | Standard MRI sequences | Specialized vascular imaging techniques |
| Preparation | Metal removal; fasting if contrast used | Same, but contrast use more likely |
| Best For | Evaluating tissue structure and organ health | Assessing vessel abnormalities and circulation issues |
| Limitations | Less precise for blood vessel imaging | Not ideal for detailed soft tissue analysis |
Primary Purpose
The core difference between MRI and MRA lies in what each test is designed to examine.
MRI (Magnetic Resonance Imaging) visualizes internal structures, including organs, bones, and soft tissue, to help detect abnormalities such as tumors or injuries.
MRA (Magnetic Resonance Angiography) specializes in imaging blood vessels to assess conditions like aneurysms, stenosis, or clots.
In short, MRI examines solid structures, while MRA examines vessels and blood flow.
Scope of Examination
MRI scans are typically broader in scope. They can be used for:
- Whole-body scans (in cancer staging or inflammatory diseases)
- Focused regional scans, such as just the spine, joints, abdomen, or brain
- Evaluations of multiple systems simultaneously
MRA, in contrast, is more targeted. It focuses on specific vascular regions, such as:
- Carotid arteries in the neck (to assess stroke risk)
- Cerebral arteries in the brain
- Coronary arteries for heart disease evaluation
- Peripheral arteries in the arms or legs
- Renal arteries to assess kidney-related vascular issues
MRI provides a detailed view of the entire body, while MRA focuses on the blood supply in specific areas.
MRA vs MRI with Contrast Agent Requirements
Both MRI and MRA can use contrast agents, but the frequency and necessity differ.
MRI may be done with or without contrast. Gadolinium-based contrast is often used to highlight abnormalities such as tumors, infection, or inflammation. However, many soft tissue or joint MRIs are performed without contrast and still provide excellent diagnostic detail.
MRA typically involves the injection of contrast, using gadolinium to enhance the visibility of blood vessels. This helps detect blockages, aneurysms, or malformations. Non-contrast MRA techniques, such as time-of-flight or phase-contrast imaging, are also an option for patients with impaired kidney function who are unable to use contrast agents.

Image Processing
While both tests use the same base technology, the post-processing methods differ.
MRI processes general tissue contrast to produce high-resolution images of internal organs, the brain, bones, and joints.
MRA employs specialized processing to isolate vascular structures, utilizing techniques such as subtraction imaging to highlight blood vessels by removing background tissue. This creates a clear map of the arterial and venous systems.
The imaging software is designed to differentiate flow dynamics and vessel anatomy, enhancing its effectiveness in vascular diagnostics.
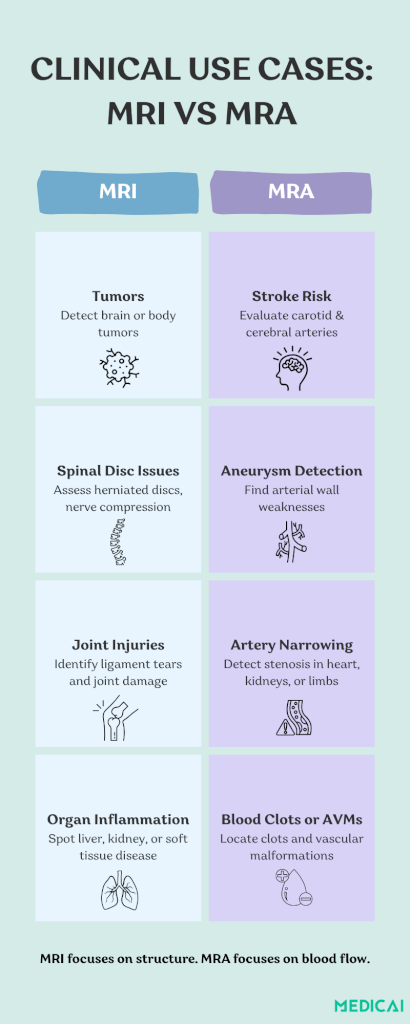
Clinical Applications
MRI is often used to diagnose:
- Brain disorders: tumors, multiple sclerosis, strokes, and structural issues
- Spinal conditions: herniated discs, nerve compression, spinal cord injuries
- Musculoskeletal injuries: ligament tears, joint degeneration, fractures
- Soft tissue masses: cysts, abscesses, and certain cancers
- Organ diseases: liver cirrhosis, kidney damage, prostate enlargement
MRA is specifically used for:
- Stroke risk assessment by evaluating carotid and cerebral arteries
- Detection of aneurysms or arterial wall abnormalities
- Identifying arterial stenosis, especially in coronary or renal arteries
- Locating blood clots and arteriovenous malformations (AVMs)
- Planning vascular surgeries or interventions like stents and bypasses
In many complex cases, MRI and MRA are ordered together to provide both structural and vascular insights.
Procedure Duration
MRI typically takes 30 to 90 minutes, depending on the size of the area being scanned, whether contrast is used, and the number of sequences required.
MRA usually takes 45 to 60 minutes. The scan may be slightly longer if contrast is involved or if multiple vascular regions are examined.
Both require the patient to lie still in the MRI machine, and sedatives may be offered for those with claustrophobia or anxiety.
Cost and Insurance
The cost of both scans depends on location, provider, insurance coverage, and whether contrast is needed.
MRI costs range widely, from $400 to $12,000 in the US. Head, spine, and joint MRIs are generally less expensive than full-body or multi-region scans.
MRA may cost more than MRI due to the use of contrast and additional image processing. Vascular specialists may also be involved in interpretation.
Most private insurance plans and public healthcare systems cover both MRI and MRA when medically necessary. Prior authorization is often required, so patients should check with their insurer beforehand.
Risks and Contraindications
Both MRI and MRA are safe and non-invasive, but there are important precautions to consider.
MRI Risks:
- Metal implants (e.g., pacemakers, aneurysm clips, cochlear implants) may be unsafe in the MRI environment due to the strong magnetic field.
- Patients with metallic tattoos, piercings, or surgical clips should notify their provider.
- People with severe claustrophobia may need medication or an open MRI option.
MRA Risks:
- Gadolinium contrast is generally safe, but in rare cases can cause allergic reactions or a condition called nephrogenic systemic fibrosis (NSF) in patients with kidney failure.
- Kidney function tests may be done before MRA to ensure contrast can be used safely.
- As with MRI, metal safety screening is required.
Similarities Between MRI and MRA
While MRI and MRA serve different diagnostic purposes, they share several similar core characteristics.
Same Technology and Machine
MRI and MRA utilize strong magnetic fields and radio waves, with no radiation involved like X-rays or CT scans. Both tests utilize the same MRI machine, so the equipment will appear and function similarly.
Similar Patient Preparation
Before either scan, patients are typically asked to:
- Remove all metal items (jewelry, watches, belts, underwire bras).
- Inform the technician about any implants, pacemakers, or metal fragments.
- Complete a medical screening form, mainly if contrast dye may be used.
- Avoid eating or drinking for a few hours prior, if contrast is involved.
Pregnant patients should inform their healthcare provider, as MRI and MRA are generally considered safe during pregnancy, especially when performed without contrast.
Painless and Non-Invasive
Both tests are non-invasive and require no recovery time. You lie on a table that moves into the MRI scanner, and the scan is painless, although it may be uncomfortable to stay still due to the loud machine noises.
Most facilities provide earplugs or headphones for the comfort of their guests.
Same Positioning and Duration
During an MRA or MRI imaging, patients lie flat and must remain still to avoid blurring the images. The scan typically lasts between 30 and 90 minutes, depending on the area being studied and whether contrast is required.
Similar Contraindications
Both MRI and MRA have shared safety precautions, particularly regarding metal and implants:
- Pacemakers and defibrillators may not be MRI-safe
- Surgical clips, metallic implants, or joint replacements need to be evaluated
- Tattoos with metallic ink or certain piercings may interfere with scanning
- Kidney issues are a concern if gadolinium contrast is needed
Interpretation and Reporting
Both scans are reviewed by a radiologist, who prepares a report for your physician. In some facilities, both MRI and MRA sequences can be performed in a single appointment, particularly for complex cases such as stroke evaluations or vascular tumors.
When to Choose MRI or MRA?
Choosing between an MRI and an MRA isn’t usually up to the patient. It’s a clinical decision made by your doctor based on what needs to be diagnosed.
When Is an MRI Recommended?
Doctors may order an MRI to:
- Investigate neurological symptoms, such as headaches, seizures, or vision changes
- Detect brain tumors, multiple sclerosis, or spinal cord issues
- Assess joint injuries, torn ligaments, or cartilage damage
- Examine internal organs for signs of infection, inflammation, or cancer
- Monitor treatment progress for chronic conditions or post-surgical healing
MRI is a versatile diagnostic tool that gives sharp anatomical detail, making it ideal for complex or unclear symptoms.
When Is an MRA Recommended?
Doctors may recommend an MRA to:
- Check for aneurysms, especially in the brain or abdomen
- Evaluate narrowed or blocked arteries (stenosis)
- Assess stroke risk or investigate the cause of a mini-stroke (TIA)
- Look for arteriovenous malformations (AVMs) or vascular tumors
- Monitor blood flow to the heart, kidneys, or limbs
- Plan surgical interventions, such as stenting or bypass surgery
Can MRI and MRA Be Done Together?
Yes, MRI and MRA are often performed together when both tissue and blood vessel information is needed. For example, a patient with a brain tumor might undergo an MRI to assess the tumor and an MRA to see if it’s affecting nearby blood vessels.
In stroke patients, doctors may order:
- An MRI to look for brain damage
- An MRA to examine the carotid arteries or cerebral vessels that supply the brain
Having both scans together provides a more comprehensive picture, enabling physicians to make better, faster decisions.
MR vs MRI: What “MR” Means in Medical Reports
MR and MRI refer to the same imaging technology, and “MRI” is the common patient-facing term for diagnostic MR scans.
MR meaning in medical reports often looks shorter, not different. “MR Brain” and “MRI Brain” usually refer to the same exam order category, with protocol details set by the radiology team.
The difference between MR and MRI comes down to wording.
- MR, umbrella term: MR refers to magnetic resonance techniques in general, imaging, angiography, venography, spectroscopy, and elastography.
- MRI, typical usage: MRI is standard anatomical imaging of organs, soft tissues, the brain, spine, and joints.
MRI vs MR confusion shows up in referrals and bills. MR names the method. MRI names the most common clinical application of that method.
MRA vs MRV: Arteries vs Veins
MRA and MRV differ by target, and the target is the vessel type.
MRA vs MRV target:
- MRA, arteries: MRA focuses on arteries and arterial flow patterns, aneurysm screening, arterial stenosis, and arterial malformations.
- MRV, veins: MRV focuses on veins and venous drainage, venous sinus thrombosis, venous outflow obstruction, venous malformations.
The difference between MRI and MRV matters when symptoms point to venous disease. MRI shows the brain tissue and surrounding anatomy. MRV shows the venous channels that drain the brain.
MRI and MRV difference in a common brain workflow looks like this.
- Brain MRI answers “Is there damage, mass, inflammation, or hemorrhage?”
- Brain MRV answers “Is venous drainage blocked or thrombosed?”
MRA vs MRI scan selection stays clinical. MRI answers structural questions. MRA answers artery questions. MRV answers vein questions.
MRI vs MRE: What Magnetic Resonance Elastography Adds
MRE is MRI plus stiffness mapping, and stiffness is the point.
The difference between MRI and MRE starts with the output. MRI produces anatomical images. MRE produces anatomical images plus a quantitative stiffness measure for targeted organs.
MRI and MRE differences are most commonly seen in liver workups. Standard liver MRI characterizes lesions and anatomy. Liver MRE estimates tissue stiffness to support fibrosis assessment and treatment tracking.
MRE ordering logic stays simple.
- MRI fits “What is it?” questions, anatomy, masses, and inflammation.
- MRE fits “How stiff is it?” questions, fibrosis risk stratification, and longitudinal monitoring.
MRE does not replace MRI. MRE extends MRI when management decisions depend on stiffness trends.
Internal Auditory Canal MRI: When MRI and MRA Both Show Up
Internal auditory canal MRI targets the hearing and balance nerves, and MRA enters the order when the question shifts to vessels.
MRI internal auditory meatus exams focus on the internal auditory canal and cerebellopontine angle. Internal auditory canal MRI is commonly used in workups for asymmetric hearing loss, vestibular symptoms, and suspected vestibular schwannoma, with contrast when the referral requests lesion characterization.
MRA pairing with internal auditory canal MRI happens when vascular anatomy could explain symptoms. Pulsatile tinnitus workups are a common example. Vascular loop evaluation and aneurysm screening fall into that category.
MRI and MRA in one appointment can share setup and scanner time. The protocol split stays clear.
- Internal auditory canal MRI answers “Is there a nerve or soft-tissue lesion?”
- Head and neck MRA answers “Is there an arterial cause or arterial abnormality near the symptomatic region?”
Radiology teams decide the exact sequence set. Referring clinicians decide the clinical question.
Conclusion
While MRI and MRA use the same technology, they serve distinctly different purposes: one examines structure, the other blood flow.
At Medicai, we’re committed to making diagnostic imaging clearer, faster, and more accessible. Whether you’re checking for joint damage or assessing stroke risk, we help providers deliver the right MRI or MRA scan at the right time.
Remember, clear images lead to better answers and better health outcomes.




