The acronyms RIS and PACS often sound like the same thing for a medical student or a new hospital administrator. They both store patient data and deal with radiology. So, why do we need two separate systems and be concerned about the difference between RIS vs PACS?
The easiest way to understand the difference isn’t to look at a feature list—it is to look at the Process Map of RIS PACS integration.
Think of the hospital as a restaurant. The RIS (Radiology Information System) is the “Front of House” (the host who takes the reservation and the waiter who takes the order). The PACS (Picture Archiving and Communication System) is the “Back of House” (the kitchen where the actual product is made and plated).
In this visual guide, we will trace the patient journey mapping step-by-step, from scan to diagnosis, to show exactly where each system takes charge.

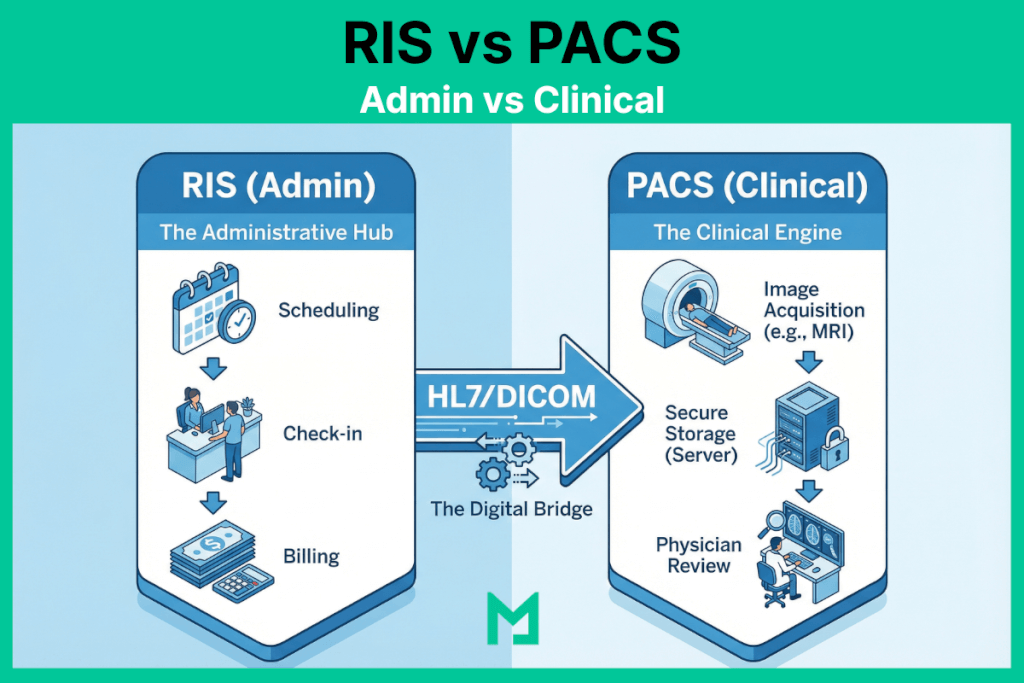
RIS vs PACS (Administrative vs. Clinical)
Here is a summary of all the differences between RIS vs PACS in a concise table.
| Feature Category | RIS (Radiology Information System) | PACS (Picture Archiving & Communication System) |
| Primary Domain | Administrative Workflow (The “Front Office”) | Clinical Diagnosis (The “Back Office”) |
| Data Type | Text-Based Data: Patient Demographics, Insurance info, Scheduling slots, Billing codes (CPT/ICD-10). | Pixel-Based Data: X-Rays, MRIs, CT Scans, Ultrasound loops, and 3D Reconstructions. |
| Key Protocol | HL7 (Health Level 7): Uses standard messaging (ORM/ORU) to talk to the EHR and Billing systems. | DICOM (Digital Imaging and Communications in Medicine): The standard for handling image storage and transmission. |
| Primary User | Schedulers, Receptionists, Billers, and Technologists (for worklists). | Radiologists, Surgeons, and Referring Physicians. |
| Core Function | “The Tracker”: Tracks the patient’s status (Arrived, Scheduled, Exam Complete, Report Distributed). | “The Viewer”: Allows the doctor to manipulate images (Zoom, Pan, Measure) to find pathology. |
| Billing Role | Critical: Generates the “Superbill,” links diagnosis codes to procedure codes, and sends claims. | Non-Existent: PACS does not handle money; it handles anatomy. |
| Integration Point | Connects to the EHR (Electronic Health Record) to pull patient history. | Connects to the Modalities (Scanners) to pull images. |
The Definitions: Administrative vs. Clinical
Before walking the path, let’s define the vehicles.
- RIS (The Manager): Handles the administrative workflow. Scheduling, billing, patient check-in, and report distribution.
- PACS (The Archive): Handles the clinical workflow. Storing images, viewing X-rays, and 3D reconstruction.
For a deeper dive into the technical architecture of the archive, read our Comprehensive Guide to PACS.
The Step-by-Step Workflow
Let’s follow a standard case: John Doe needs a Chest X-ray.
Step 1: The Order (Domain of RIS)
The Actor: Ordering Physician / Scheduler The Action: John’s doctor places an order in the EHR. This order flows into the RIS.
- What happens here: The RIS checks John’s insurance eligibility, schedules the appointment, and generates a unique Accession Number.
- Why it matters: Without the RIS, the radiology department wouldn’t know John is coming.
Step 2: The Acquisition (The Handshake)
The Actor: Technologist The Action: John arrives. The technologist queries the “Modality Worklist” on the X-ray machine.
- What happens here: The X-ray machine pulls John’s demographics from the RIS but prepares to send the actual images to the PACS.
- The Critical Link: If the data here doesn’t match, you get “broken links.” (See our guide on Preventing Data Mismatches).
Step 3: The Image Storage (Domain of PACS)
The Actor: The Server / Archive The Action: The scan is complete. The heavy image files—encoded in the DICOM standard—are transmitted to the PACS server.
- What happens here: The PACS acts as the vault. It stores the pixels and ensures they are available for viewing anywhere in the hospital.
Step 4: The Diagnosis (Domain of PACS)
The Actor: Radiologist The Action: The radiologist sits at their workstation. They open the study in the DICOM Viewer.
- What happens here: This is pure clinical work. The radiologist uses tools like Window/Leveling and measurement calipers to analyze the image. They aren’t looking at billing codes; they are looking at anatomy.
Step 5: The Report (The Synchronization)
The Actor: Radiologist / Transcription The Action: The radiologist dictates their findings: “Clear lungs, no pneumonia.”
- What happens here: This is where it gets tricky. The diagnosis (text) is created in the PACS (or a dictation system), but it must be sent back to the RIS so the bill can be generated and the result sent to John’s doctor.
The Future: Do We Still Need Both?
Historically, you needed an RIS from Vendor A and a PACS from Vendor B. This required complex HL7 integration to keep them talking.
Today, the lines are blurring. Modern, cloud-native platforms are moving toward a “Unified Radiology Platform” model.
By using a Vendor Neutral Archive (VNA) approach, modern systems can store both administrative data (RIS) and image data (PACS) in a single, seamless database. This eliminates the “swivel chair” effect and ensures that the radiology workflow diagram is a straight line, not a tangled web.
From Scan to Diagnosis
Understanding RIS vs. PACS is effectively understanding the difference between the “Ticket” and the “Meal.”
The RIS ensures the patient reaches the scanner and the bill is paid. The PACS ensures the doctor can see inside the patient to find the cure. Both are essential, but the future belongs to platforms that can do both without forcing users to switch screens.




