What if the very tools designed to support radiologists are limiting their potential?
A one-size-fits-all approach doesn’t work in medical imaging because it cannot accommodate real patients and radiologists’ diverse anatomical, pathological, and workflow needs. Standard protocols ignore critical variables like body type, disease complexity, and user preferences, leading to inefficiencies, diagnostic gaps, and burnout.
Let’s explore why personalization is no longer optional and how adaptive imaging systems are shaping the future of radiology.

Why a One-Size-Fits-All Approach Is Problematic in Medical Imaging
Medical imaging is vital for diagnosis and treatment, but standardized protocols often clash with real-world patients’ biological and clinical diversity.
While standardization has historically improved interoperability and consistency, especially with the development of DICOM and national dose protocols, it’s becoming clear that what works well for the “average patient” often fails the individual one.
Let’s explore why one size does not fit all in radiology.
Anatomical Diversity
No two human bodies are exactly alike. Organ size, shape, positioning, and vascular structure vary significantly, even among healthy individuals. Standardized imaging protocols, by definition, are built on population averages, which means they often don’t perform well at the margins.
For example, modifying CT protocols is crucial for specific patient populations.
- Obese patients might need increased exposure, scan time, or special reconstruction.
- Children are susceptible to overexposure in standard adult settings.
- Rare anatomies or vascular anomalies may necessitate customized views for accurate diagnosis.
Rigid protocols leave little room for these adjustments unless technologists break from the standard—a risky and inconsistent workaround.
Demographic and Health Disparities
Imaging inequities also persist across race, age, gender, and socioeconomic status:
- Black patients get less diagnostic imaging than white patients with similar symptoms.
- Women receive less tailored breast cancer screening despite higher use due to density.
- Children and the elderly often undergo standard adult imaging protocols due to operational demands, despite needing different approaches.
While standardization offers efficiency, its assumption of equal access, compliance, and biological presentation across diverse populations can exacerbate existing inequalities.
Pathological Variability
Disease does not follow a script. Even well-known conditions like pneumonia, stroke, or cancer can present atypically based on comorbidities, stage, or immune status.
Standardized protocols, optimized for common patterns, often fail to:
- Detect early, subtle changes
- Differentiate between similar-appearing pathologies (e.g., pneumonia vs. atelectasis)
- Adjust dynamically when clinical suspicion evolves
Radiologists often require specialized sequences, alternative views, or multi-modality inputs in these scenarios.
Operational Barriers
Even with the best intentions, real-world imaging departments struggle to maintain protocol consistency. Factors like:
- “Protocol drift”—unauthorized tweaks made over time
- Technical limitations—older machines or varying vendor platforms
- Staff shortages and turnover
This leads to unintentional deviations that undermine standardization itself.
Paradoxically, forcing uniformity can result in fragmented implementation, where protocols appear consistent on paper but vary significantly in practice.

Individual Patient Needs Can’t Be Mass-Produced
Patients bring diverse lived experiences, languages, and personal preferences. Some may not speak the local language, while others may refuse contrast agents for religious reasons. Children and elderly patients with dementia often struggle with breath-holding instructions or lengthy scans.
Standard protocols typically do not account for:
- Cultural comfort
- Physical limitations
- Psychological states
- Access barriers in rural or resource-limited settings
Imaging protocols must be adaptable to anatomy and disease and to the human context in which care is delivered to serve all patients equitably.
The Standard Workflow Model: Designed for Speed, Not Precision
One-size-fits-all imaging protocols overlook patient diversity, and the current workflow in radiology departments exacerbates this issue. Designed for speed and volume, the system prioritizes quick processing over adaptability and personalization.
While standardization aimed for consistency, it has created a high-pressure environment that compromises diagnostic clarity and clinician collaboration.
Assembly-Line Mentality in Modern Radiology
According to a study, radiologists are increasingly seen as image processors rather than clinical decision-makers. The emphasis is on clearing queues, not understanding the nuanced needs of the case or the patient.
The result?
A culture where quantity is rewarded over quality, and where the software reflects that reality.
Imaging platforms are built for standard throughput, not tailored care. Workstations often lack flexibility, forcing every user through the same rigid steps regardless of the modality, urgency, or user preference.
This disconnect hampers the quality of care and contributes to professional burnout, as radiologists feel like they’re racing against the system rather than working with it.
Workflow Friction Points That Compromise Care
Even the most experienced radiologists are slowed down by systems not designed to support complex, individualized care. Some of the most common bottlenecks in traditional workflows include:
- Inaccessible Prior Exams: Accessing historical images should be seamless, but delays and poor integration complicate detecting subtle changes, vital in oncology, neurology, and trauma cases.
- Poor Hanging Protocols: Display settings that don’t align with the user’s preferred layout or the case type result in extra clicks, reordering, and visual clutter.
- Interface Inefficiencies: Buried tools, confusing navigation, and an unresponsive UI cause cognitive overload, resulting in reduced efficiency and missed details, not due to a lack of expertise, but because of technological drag.
These issues highlight the risks of prioritizing system rigidity over clinical flexibility, especially as diagnostic demand grows and imaging plays a larger role in care pathways.

Cases Against Uniform Systems For Radiologists
Every patient is unique, and so is each radiologist’s approach to thinking, working, and interpreting images. Standard imaging procedures often overlook these differences in how radiologists analyze images.
Human Variability Meets System Rigidity
Radiology is not a purely technical field—it’s a human one. Radiologists bring their personalities, strengths, habits, and stress responses into every case they read. These differences include:
- Variations in visual perception and image navigation strategies
- Different levels of tech fluency and experience with digital tools
- Preferences for interface layout, reporting workflows, and annotation tools
- Differences in motor skills, cognitive pacing, and fatigue thresholds
When systems fail to adapt to user-specific factors, radiologists must adhere to rigid workflows that can hinder their performance. This can lead to a mismatch between their preferred work methods and system expectations.
Stress, Fatigue, and the Cost of Inflexibility
Radiology is a demanding specialty that requires long hours and complex cases, leading to cognitive load and emotional fatigue. However, most imaging systems do not consider the radiologist’s focus, mental bandwidth, or emotional stress.
That’s when the concept of affective computing was introduced.
Affective computing is technology that responds to human emotions and stress. Imagine a platform that detects cognitive overload, reduces non-essential notifications, simplifies the interface, or prioritizes decision support features.
Uniform Tools in a Specialized World
Ironically, the tools remain one-dimensional as radiology becomes more subspecialized, like neuroradiology and musculoskeletal. Whether interpreting trauma CTs or breast MRIs, the interface doesn’t change, despite the differing tasks and cognitive demands.
An adaptive platform would recognize this. It would change based on:
- The radiologist’s specialty and preferences
- The type of exam being read
- The user’s real-time performance and stress patterns
This level of personalization is not just a user experience improvement—it’s a clinical performance multiplier.
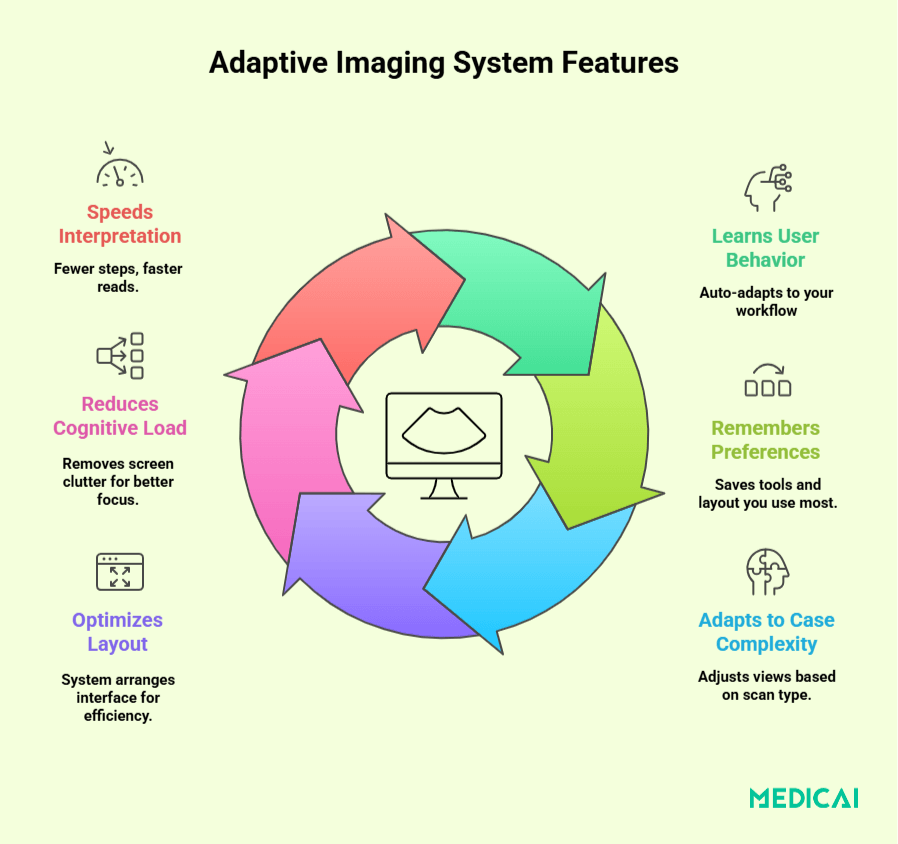
What Adaptive Imaging Systems Look Like
What does the solution look like if rigid protocols and standardized platforms are the problem? The answer lies in adaptive imaging systems—technologies designed for cases and those managing them.
User-Specific Profiles That Learn and Adjust
The foundation of an adaptive system is its ability to recognize and respond to the individual radiologist. This isn’t about changing button colors or saving monitor presets—it’s about building a smart profile that evolves with the user.
These systems capture:
- Preferred viewing sequences or image arrangements
- Frequently used tools and shortcuts
- Speed and style of image navigation
- Patterns of decision-making or hesitation
Over time, the platform adapts. It knows your workflow, anticipates what you need before you ask, and creates a working environment that feels tailored, not forced.
Real-Time Responsiveness to Cognitive Load
True adaptability also means responding to more than clicks and settings. It means recognizing when the radiologist is stressed, overwhelmed, or distracted and offering support, not more noise.
Affective computing makes this possible. Imagine a platform that detects:
- Slower-than-normal image navigation
- Missed keystrokes or erratic input
- Extended time on specific views
- Changes in cursor speed or movement
From this, the system can make smart, compassionate adjustments—pausing pop-ups, simplifying menus, surfacing helpful tools, or offering AI assistance for high-difficulty tasks.
This isn’t about replacing radiologists. It’s about giving them a smarter co-pilot that knows when to help and when to get out of the way.
Task-Specific Adaptation That Follows Clinical Context
Adaptability shouldn’t stop at the user. It should extend to the type of case being read.
For example, a screening mammogram may call for rapid, side-by-side comparisons, or a multi-trauma CT may require full-body navigation tools and quick toggling between bone and soft tissue windows.
Adaptive systems provide tailored workflows based on modality, clinical suspicion, urgency, and image complexity, minimizing cognitive load and helping radiologists focus on interpretation rather than interface management.

Benefits of Moving Beyond One-Size-Fits-All
Shifting from standardized to adaptive imaging systems enhances diagnostic accuracy, workflow efficiency, and patient safety. When technology aligns with radiologists’ needs, it positively impacts the entire healthcare system.
Improved Diagnostic Accuracy
Radiologists rely on patterns and details in images, but poor interfaces and navigation can lead to mistakes. Adaptive systems reduce friction and preserve focus by aligning with each radiologist’s natural reading style and visual preferences.
It can lead to:
- Fewer missed findings
- More confident interpretations
- Greater consistency across complex or borderline cases
Increased Workflow Efficiency
Adaptive systems save time by:
- Automatically surfacing preferred tools or sequences
- Reducing redundant steps
- Minimizing interface overload
- Preloading historical comparisons or relevant priors
- Supporting decision-making through AI-assisted triage
This minimizes cognitive switching and fatigue, allowing radiologists to work faster with greater clarity and less stress. The result is fewer delays, workarounds, and missed steps that waste time.
Better Patient Outcomes
When intelligent, responsive systems support radiologists, patients benefit in real ways:
- Faster diagnoses mean earlier treatment.
- More accurate interpretations reduce the need for repeat imaging or follow-ups.
- Tailored imaging increases safety by reducing unnecessary radiation or contrast use.
- Smarter workflows minimize wait times and improve access, especially in resource-limited settings.
The Role of Industry Innovators
Addressing the limitations of one-size-fits-all imaging demands tech innovation that truly understands radiology. Emerging platforms like Medicai are rethinking how radiologists engage with their tools.
From Static Tools to Adaptive Environments
Traditional systems were built for volume and standardization. Today’s innovators are building platforms prioritizing intelligence, flexibility, and user experience.
These adaptive platforms:
- Learn from individual user behavior and preferences
- Tailor interfaces to match specialty, modality, and case complexity
- Reduce visual and cognitive overload with context-aware tools
- Enable real-time collaboration across roles without disrupting workflow
It’s a shift from rigid infrastructure to dynamic, responsive design that prioritizes the radiologist’s needs.
Building for Real-World Workflow
The most forward-thinking solutions integrate:
- Smart DICOM viewing with personalized layout memory
- Secure, cross-team collaboration features
- AI-assisted triage and guidance tools that enhance—not replace—human insight
- Modular design that works across systems, specialties, and legal or clinical contexts
True personalization in imaging starts with understanding the user. The most impactful innovations adapt not just to patient complexity but also to the way radiologists work best.
Conclusion
Standardized imaging is limited; today’s radiologists require adaptable tools for patient complexity, user variability, and clinical context. A one-size-fits-all approach can lead to inefficiency, missed findings, and burnout.
The future is in intelligent systems like Medicai, which evolve with users to enhance collaboration and support precise decision-making. Our adaptive platform helps healthcare teams to provide faster, smarter, and safer care.



