What if every healthcare provider had instant access to a patient’s complete medical history, regardless of where they received care?
Functional interoperability makes this possible. Here, I have explored the transformative potential of interconnected healthcare systems, exploring the benefits, challenges, and solutions for achieving this vision.
If you’re a healthcare professional, facility executive, or owner seeking to optimize care delivery and streamline operations, discover how functional interoperability can revolutionize your organization.

What Is Interoperability in Healthcare?
Interoperability in healthcare refers to the ability of different health information systems, devices, and applications to connect and communicate with each other securely and seamlessly. This allows for the efficient and accurate exchange of electronic health information (EHI) among various stakeholders, including:
- Researchers: Analyzing data to improve treatments and outcomes
- Healthcare providers: Hospitals, clinics, pharmacies, labs
- Patients: Individuals accessing their own health records
- Payers: Insurance companies and government agencies
- Public health organizations: Monitoring disease outbreaks and trends
Examples of Interoperability in Healthcare
Here are some examples and cases of interoperability in healthcare.
Sharing patient records between hospitals and clinics: Allows providers to access a patient’s complete medical history, including allergies, medications, and test results.
Connecting pharmacies with prescribers: Enables electronic prescriptions and reduces medication errors.
Integrating patient portals with EHRs: Empower patients to access their health information, schedule appointments, and communicate with providers.
Public health reporting: Facilitates the electronic reporting of infectious diseases and other health data to public health agencies.
Why is Interoperability Important in Healthcare?
Interoperability is an essential aspect of the healthcare industry. It allows healthcare providers to access and exchange important patient information quickly and accurately, reducing errors, improving patient outcomes, and enhancing the overall efficiency of the healthcare system.
Let’s check the benefits of interoperability in detail.
Improved patient care
Interoperability provides clinicians with a complete picture of a patient’s health history, regardless of where they received care. It enables better-informed decision-making, reduces medication errors, and avoids unnecessary tests.
Enhanced care coordination
Facilitates communication among different providers involved in a patient’s care, leading to more coordinated and efficient treatment plans.
Increased efficiency and cost savings
Streamlines administrative processes reduces duplicate testing, and minimizes paperwork.
Empowered patients
Gives patients greater access to their health information, allowing them to actively participate in their care and make informed decisions.
Public health advancements
Supports population health management, disease surveillance, and research efforts.
Barriers to Interoperability in Healthcare: The Interoperability Challenges
The challenges of interoperability are multifaceted and require an integrated approach to resolve.
Technical barriers
Different systems may use various standards, protocols, and data formats, making it difficult to exchange information seamlessly.
Security and privacy concerns
Protecting sensitive patient data during exchange requires robust security measures and compliance with regulations like HIPAA.
Organizational and financial barriers
Healthcare organizations may have different priorities, resources, and incentives, challenging collaboration and data sharing.
Lack of standardization
While progress has been made, the lack of universal standards for health data exchange can hinder interoperability.

How to Improve Interoperability in Healthcare?
Improving interoperability in healthcare is a multifaceted challenge that requires a collaborative effort from various stakeholders. Here are some key strategies:
Embrace Standardized Data Formats and Protocols
- Adopt FHIR: Fast Healthcare Interoperability Resources (FHIR) is a modern standard that is gaining widespread adoption. It uses web-based APIs, making it easier for different systems to communicate.
- Utilize existing standards: Leverage established standards like HL7 v2 and CDA for specific use cases.
- Promote data harmonization: Encourage using common data elements and terminologies to ensure consistent meaning across systems.
Prioritize Data Security and Privacy
- Implement robust security measures: Employ encryption, access controls, and audit trails to protect patient data during transmission and storage.
- Ensure HIPAA compliance: Adhere to all relevant regulations and guidelines for protecting patient privacy.
- Build trust: Establish clear policies and procedures for data sharing and access, and be transparent with patients about how their data is used.
Foster Collaboration and Information Sharing
- Encourage cross-organizational partnerships: Facilitate communication and data exchange between different healthcare providers, payers, and public health agencies.
- Establish health information exchanges (HIEs): Support the development and use of HIEs to facilitate secure data sharing within a region or community.
- Promote data liquidity: Remove barriers to data sharing and ensure that information flows freely to where it’s needed most.
Invest in Technology and Infrastructure
- Upgrade legacy systems: Modernize outdated systems to support interoperability standards and technologies.
- Utilize cloud-based solutions: Cloud platforms like PACS can offer scalability, flexibility, and cost-effectiveness for data storage and exchange.
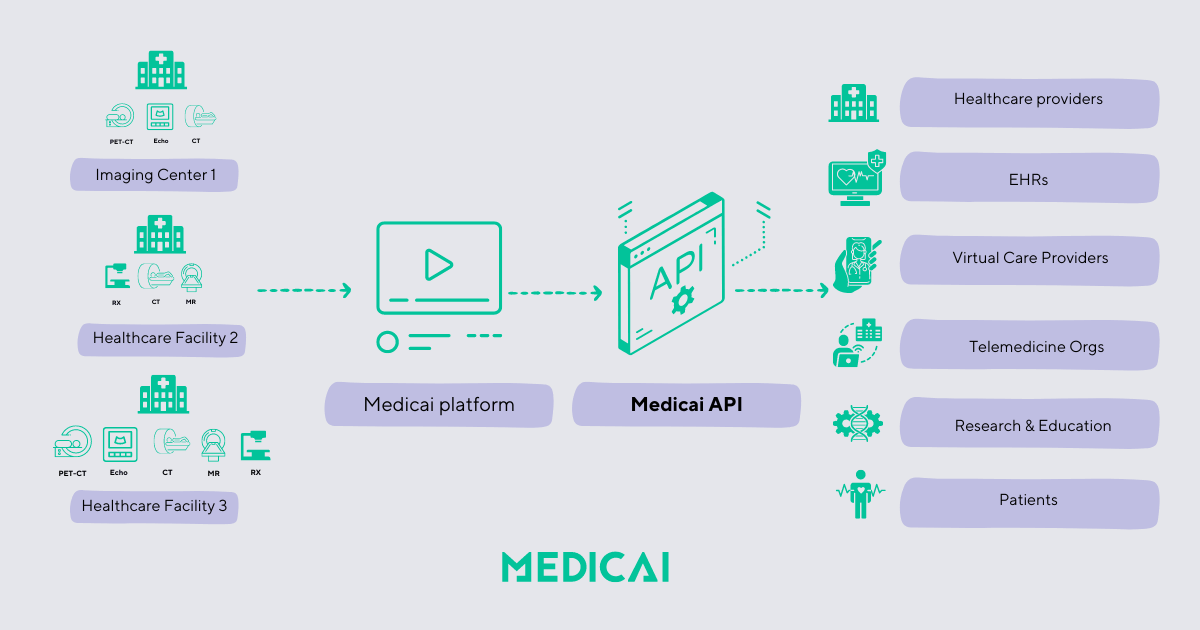
- Explore API-driven approaches: APIs enable seamless communication between different applications and systems.
Empower Patients and Providers
- Provide patient access to data: Give patients easy access to their own health information through patient portals and other tools.
- Educate and train the workforce: Ensure that healthcare professionals understand the importance of interoperability and are trained to use interoperable systems effectively.
- Promote digital health literacy: Empower patients to use digital tools to manage their health and participate in their care.
Support Ongoing Innovation and Research
- Monitor and evaluate progress: Track the impact of interoperability initiatives and make adjustments as needed.
- Invest in research and development: Support the development of new interoperability solutions and technologies.
- Pilot and test new approaches: Encourage experimentation and innovation in real-world settings.
Types of Interoperability in Healthcare
Interoperability in healthcare isn’t a one-size-fits-all concept. It’s a multi-layered framework that allows different health information systems to communicate and exchange data in increasingly complex ways. Think of it like a pyramid, each level building upon the one below it. Let’s explore these levels:
Foundational Interoperability: The Base Layer
This is the most basic level, ensuring that systems can simply connect and exchange data. Imagine two people speaking different languages but having a basic translator app. They can exchange basic information, but nuances might be lost. In healthcare, this means systems can send and receive information, but it might not be usable without further processing.
Example: A hospital sends a patient’s lab results to a primary care physician’s office.
Structural Interoperability: Organizing the Exchange
Building upon the foundation, structural interoperability standardizes the format of data exchange. This ensures that the receiving system can understand and interpret the information correctly. Now, our language analogy includes a shared grammar book, making sentences clearer.
Example: Using HL7 FHIR to structure patient data, ensuring consistency across different EHR systems.
Semantic Interoperability: Sharing Meaning
This is where things get really interesting. Semantic interoperability ensures that all systems understand the meaning of the data. Our language analogy now includes a shared dictionary, ensuring everyone understands the meaning of words. In healthcare, this means using standardized terminologies and codes so that everyone interprets data similarly.
Example: Using SNOMED CT to represent medical diagnoses, ensuring that “diabetes” in one system means the same thing in another.
Organizational Interoperability: The Human Factor
This level goes beyond technology and addresses the human factors involved in data exchange. It focuses on policies, workflows, and governance to ensure seamless and secure information sharing between different organizations. This is like establishing cultural norms and etiquette for our language speakers.
Example: Establishing agreements between hospitals and clinics to share patient data for care coordination while adhering to privacy regulations.
Conclusion
Functional interoperability in healthcare is no longer a futuristic concept but a present-day necessity.
By embracing standardized data formats, prioritizing security, and fostering collaboration, healthcare organizations can unlock the true potential of interconnected systems. This translates to better care coordination, reduced medical errors, empowered patients, and a more efficient and effective healthcare ecosystem.
While challenges remain, functional interoperability’s benefits far outweigh the costs, paving the way for a brighter future for both patients and providers. Now is the time to invest in the solutions that will transform your organization and contribute to a more connected and collaborative healthcare landscape.




