The landscape of breast cancer detection is shifting.
While much of the public health focus remains on women over 50, recent data suggests that younger women represent a substantial and consistently high-risk portion of the patient population.
For MedTech providers and radiology departments, this demographic shift necessitates more vigilant imaging protocols and the adoption of advanced technologies, such as Mammography PACS, to detect aggressive cancers early.

The Changing Landscape of Breast Cancer Detection
For many years, the clinical “gold standard” for screening focused on the post-menopausal demographic.
However, an 11-year study (2014–2024) conducted at Elizabeth Wendy Breast Care reveals a different reality in community breast facilities. Women aged 18 to 49 comprise approximately 21% to 25% of the annual patient volume.
This is not a small subset; it is a quarter of the total patient base. More importantly, the absolute number of breast cancers found in this cohort has remained stable over the last decade, highlighting that younger women are a “substantial portion” of the breast cancers identified in clinical settings.
To manage this volume effectively, facilities must look beyond traditional workflows and embrace high-performance digital infrastructure.
Key Data: Understanding the “Young Patient” Cohort
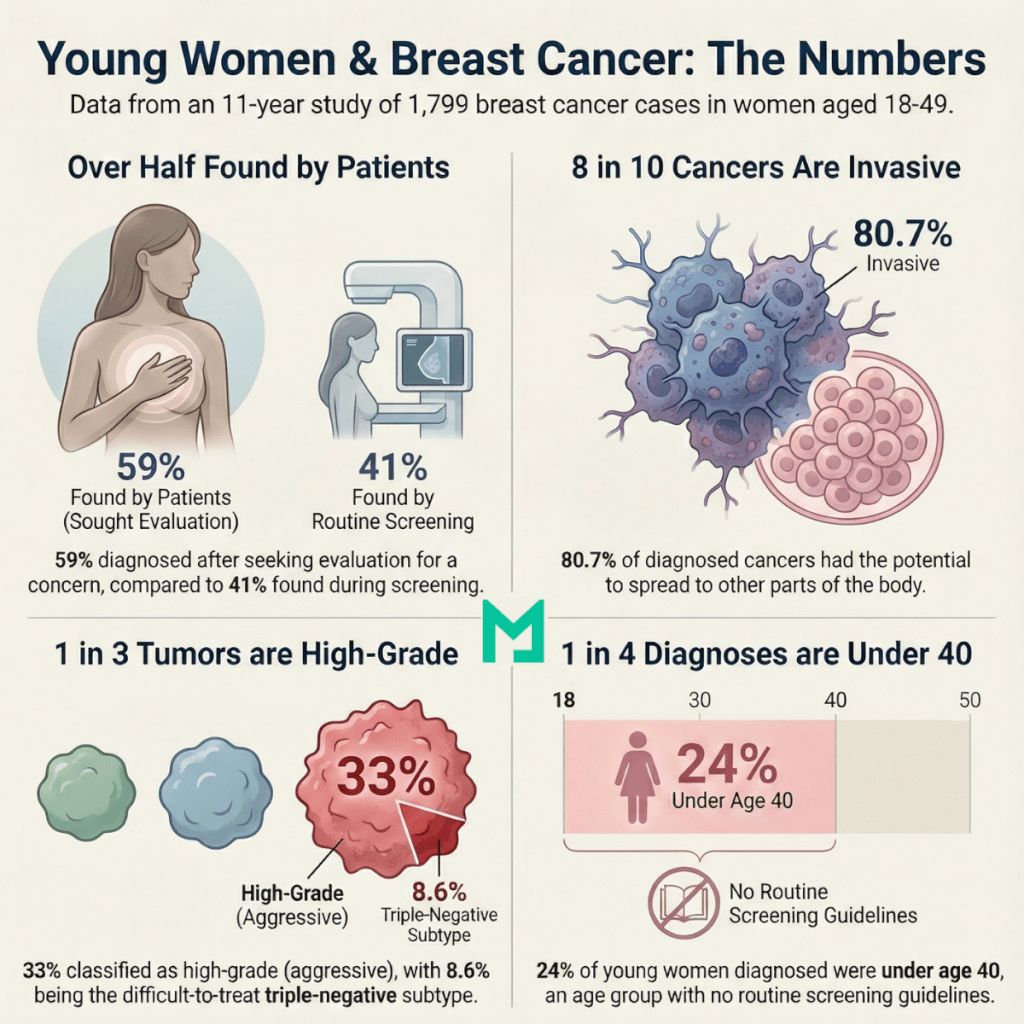
To understand why advanced imaging is necessary, we must look at the specific characteristics of cancers found in women under 50. The Elizabeth Wendy Breast Care study reviewed 1,799 breast cancers diagnosed in 1,290 women within this age group.
The Screening vs. Diagnostic Gap
One of the most telling statistics from the study is how these cancers are found. Only 41% of cancers were detected through routine screening mammography, while a significant 59% were diagnostic.
This means the majority of these young patients did not find their cancer through a scheduled check-up; they presented with symptoms that required immediate, focused evaluation.
Aggressiveness of Cancers
The study characterizes many of these cases as “bad players” due to their aggressive nature:
- Invasive Cancers: 80.7% of the total cancers found in this group were invasive.
- High-Grade Tumors: 33% (one-third) of the cases were high-grade, indicating fast-growing cells.
- Triple Negative: 8.6% were triple-negative, a subtype historically more difficult to treat and requiring rapid identification.
- Tumor Size: The average tumor size for invasive cancers was 2.2 cm, while non-invasive (DCIS) cancers averaged 2.7 cm.
The Under-40 Challenge
Perhaps most concerning is the data regarding women under 40. This group accounted for 24% of the cancers in the study, yet they are a demographic for which standard screening guidelines do not currently exist.
For these women, “vigilance” is not just a recommendation; it is a clinical necessity.
The Need for “Vigilant Imaging Protocols”
The study concludes that, because these younger patients often present with aggressive, invasive disease, radiologists must be “vigilant in imaging protocols” to identify these cases promptly.
This is where a Mammography PACS (Picture Archiving and Communication System) becomes an indispensable tool.
- High-Resolution Precision: Given that invasive tumors in this study averaged 2.2 cm, the ability to see micro-calcifications and subtle architectural distortions is vital. A specialized PACS provides the high-fidelity rendering required for dense breast tissue, which is common in younger women.
- Multi-Modality Integration: Since 59% of these cases are diagnostic, radiologists often need to compare mammograms with ultrasounds or MRIs. A modern PACS allows for a side-by-side, seamless comparison of different imaging modalities, speeding up the time to diagnosis for “high-grade” tumors.
- Historical Data Access: The study tracked data over 11 years. A cloud-based PACS ensures that a patient’s prior imaging is always available, enabling longitudinal tracking of even the slightest changes in breast tissue.

Supporting the Transition to Earlier Screening
The findings from Elizabeth Wendy Breast Care support a growing call in the medical community for earlier or more intensive screening for high-risk, younger populations. When 33% of cancers in this age group are high-grade, waiting until age 50 for a first mammogram may result in missing critical windows for treatment.
By utilizing a MedTech solution like Medicai, facilities can better manage the influx of younger patients. A streamlined PACS reduces the administrative burden of handling “diagnostic” cases, which are often more complex and time-consuming than routine screenings.
It allows the radiologist to focus on the “bad players”—the aggressive triple-negative and invasive cancers that require immediate intervention.
Empowering Radiologists to Save Younger Lives
The data is clear: women under 50 represent a significant percentage of the breast cancer volume, and the cancers they develop are often aggressive and invasive. The absolute stability of these numbers over the last 11 years proves that this is not a temporary trend, but a consistent clinical reality.
To fight these “bad players” effectively, healthcare providers need more than just hope; they need vigilant imaging protocols and the best tools available. Medicai’s Mammography PACS provides the infrastructure necessary to detect, analyze, and manage these high-stakes cases with the speed and accuracy they demand.




