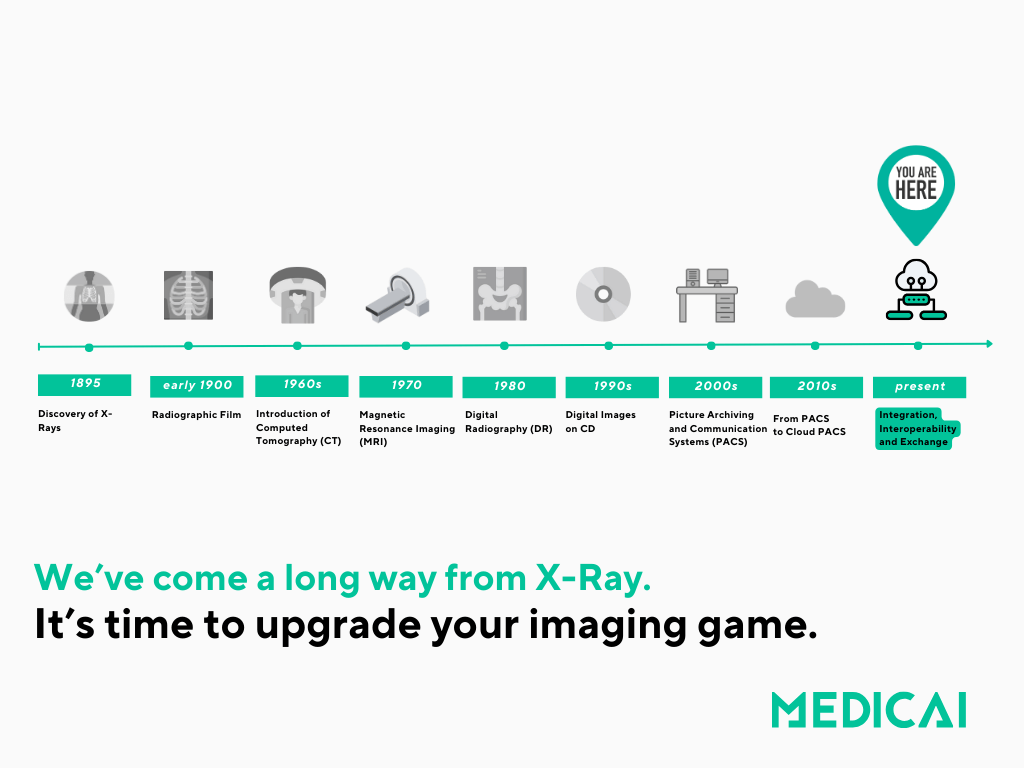
Medical imaging data (from X-rays, CT scans, ultrasounds, MRIs, and digital pathology) was once primarily stored in physical formats, such as film. Today, however, these images are captured, managed, and stored digitally using advanced systems, improving accessibility and sharing capabilities.
This transformation has significantly enhanced the ability to provide accurate diagnoses and tailor therapy plans to individual patients.

History and Evolution of PACS
The history and evolution of Picture Archiving and Communication Systems (PACS) is marked by major technological milestones, industry collaborations, and the drive to solve practical challenges in medical imaging.
Early Development
- 1970s: The roots of PACS date back to the early 1970s, when the first basic systems were conceptualized to manage digital images from new imaging modalities, such as CT. Dr. Richard J. Steckel created one of the earliest basic PACS in 1972.
- 1980s: The principles of PACS were openly discussed at radiology conferences, and formal research initiatives began. Early implementations aimed to relieve the burden of film storage, retrieval, and sharing, which were time-consuming and error-prone.
The Move Toward Standardization
- 1982–1985: The American College of Radiology (ACR) and the National Electrical Manufacturers Association (NEMA) formed a joint committee to create common standards for digital image transfer and device communication. This led to the release of the first ACR-NEMA standard in 1985, which specified data formats and hardware interfaces.
- 1993: The DICOM (Digital Imaging and Communications in Medicine) standard was introduced, building on ACR-NEMA. DICOM provided vendor-neutral, standardized protocols for image storage, communication, and management—becoming foundational for all modern PACS.

Major Milestones & Evolution
- 1982: The first large-scale PACS implementation was installed at the University of Kansas, representing a shift from isolated experiments to enterprise-level imaging management.
- Early 1990s: Hammersmith Hospital in London became the UK’s first “filmless” hospital, thanks to extensive government funding and leadership by Dr. Harold Glass. Around the same time, U.S. military medical centers introduced PACS as part of large federal programs.
- 1990s–2000s: Advances in networking (transition to Ethernet and the Internet), expansion of DICOM, and dramatic increases in computing power allowed PACS to support a broader range of image types (CT, MRI, PET, etc.), facilitate telemedicine, and enable integration with Radiology Information Systems (RIS) and Hospital Information Systems (HIS).
Key Technological Drivers
- Digital Imaging: The adoption of computed radiography (CR) and digital radiography (DR) has provided high-resolution images suitable for electronic storage and rapid retrieval.
- Networking: Evolution from proprietary and slow networks to fast Ethernet and then internet-based protocols broadened the reach and scalability of PACS, enabling multi-site and even global image exchange.
- Standardization: The emergence of DICOM solved the challenge of cross-vendor interoperability, making it possible to integrate images from any digital modality and setting the stage for enterprise-level PACS.
The Modern Era (2000s–Present)
Vendor Neutral Archives (VNA): As PACS matured, limitations tied to proprietary formats or systems led to the rise of VNAs, which emphasize interoperability beyond DICOM, integrating other medical data types and further decoupling storage from vendor lock-in.
Cloud Adoption: From the 2010s onward, cloud-based PACS deployments enabled scalable, flexible, and cost-effective storage, offering rapid disaster recovery and supporting telehealth and remote diagnostics.
Integration with EHRs: PACS has become embedded within electronic health record (EHR) systems, streamlining clinical workflows and enhancing patient care.
Interoperability and Data Sharing
Interoperability and data sharing have also become crucial aspects of modern PACS. With the growing emphasis on value-based care, there is an increasing need for patient data to be shared seamlessly between different healthcare facilities, whether it’s a specialist or an external imaging center.
To achieve this, PACS has adapted by supporting standardized protocols like DICOM (Digital Imaging and Communications in Medicine) and integrating with Health Information Exchanges (HIEs), making patient imaging data more accessible across diverse healthcare networks.
These changes have shifted PACS from a primarily radiology-focused tool into a central component of an integrated healthcare IT ecosystem, where data is available on demand, regardless of where the patient has been treated. This evolution ultimately supports a more holistic view of patient health, improves outcomes, and enhances the patient experience through more connected and timely care.
Challenges in the Evolution of Medical Imaging: Balancing Portability with Security and Integration
Overcoming Data Silos and Transitioning Beyond CD-Based Systems
At the heart of this issue is the existence of data silos, where imaging data generated by various modalities and healthcare institutions reside in isolated repositories, often incompatible with one another.
On-premise systems offer decent security, ensuring that only people inside the organization could access the data. However, this fragmentation makes it difficult for clinicians in separate organizations to work together, which results in inefficiencies, redundant procedures, and suboptimal patient outcomes.
The practice of handing over imaging data on a CD further complicates matters, creating physical barriers to accessibility, both for patients and their physicians.
This fragmentation makes it difficult for clinicians in separate organizations to work together, resulting in inefficiencies, redundant procedures, and suboptimal patient outcomes.
CDs also pose security risks, as they can be lost, stolen, or damaged, compromising patient data privacy. For patients, accessing their own medical information becomes cumbersome, limiting their ability to share data with different healthcare providers effectively, and ultimately affecting their quality of care.
The decentralization of healthcare services requires access to medical data (including imaging) from different locations
As healthcare shifts towards more distributed models—such as outpatient centers, telehealth, virtual care—the need for comprehensive and efficient data sharing becomes crucial.
Clinicians, regardless of their physical location, must be able to access, analyze and collaborate on medical records and imaging results in real time to provide timely and effective patient care. This connectivity not only ensures continuity of care but also reduces the risk of diagnostic delays.
The Dire Need for Imaging Data Access in Complex Care
The dire need for access to imaging data is becoming increasingly apparent in complex care as clinicians deal with multifaceted patient cases and conditions. In complex care scenarios, having access to complete data is essential for treatment planning, making well-informed decisions, and tracking the progression of disease.
Clinicians rely on imaging data to clarify anatomical details, recommend treatment and evaluate treatment efficacy while managing chronic illnesses, rare diseases, or sophisticated surgical operations.
Clinicians have a difficult time providing individualized, evidence-based treatment that caters to the particular requirements of each patient if they do not have easy access to imaging data. Therefore, improving access to imaging data is essential to achieving better results and higher standards of care in complex medical circumstances.
To address these challenges, there is an urgent need for a paradigm shift towards imaging data exchange at scale.
What would be required for an imaging data exchange system to operate effectively on a large scale?
Fundamentally, this means building APIs and exchange protocols to seamlessly transmit imaging data across disparate platforms and systems.
Initiatives such as the Digital Imaging and Communications in Medicine (DICOM) standard have laid the foundation for interoperability in medical imaging.
Yet, gaps remain in semantic interoperability, data normalization, and ontology mapping.
Gaps and challenges in the DICOM standard
Semantic Interoperability: inconsistent use of DICOM Tags
DICOM defines a vast set of tags (attributes) to describe medical images and associated metadata, such as patient information, modality, and imaging protocols. However, inconsistent use of these tags across different vendors, institutions, or even departments within the same institution can create challenges.
Example: The same anatomical location or imaging protocol might be coded differently by different imaging devices, leading to variability in how data is interpreted.
This inconsistency can lead to misinterpretation of images and their associated metadata when exchanged between systems.
Lack of Integration with EHR Systems
DICOM is highly focused on medical imaging, while electronic health records (EHRs) contain a broader range of patient data, such as lab results, medications, diagnoses, and clinical notes. DICOM systems often lack deep integration with EHR systems, leading to disjointed access to clinical data.
Example: A radiologist might not be able to easily access a patient’s complete clinical history from the imaging workstation because the DICOM data is not fully interoperable with the EHR system.
Lack of access to comprehensive patient data can result in suboptimal clinical decisions or the need for manual data entry, increasing the risk of errors.
The Need for Regulating PACS Vendors
PACS vendors have been overwhelmingly under-regulated, a key factor contributing to the persistence of data silos and the challenges associated with accessing medical imaging across healthcare systems.
PACS vendors have long operated with minimal regulatory oversight, which has led to proprietary systems that lock data into isolated repositories, hindering seamless sharing.
A more balanced approach that includes regulating PACS vendors and ensuring their platforms are open and interoperable is essential. Only then can we break down the silos and facilitate easy access to medical imaging data across different locations, empowering both healthcare providers and patients.
New Rule Introduces Imaging Criteria for EHR Certification
A new proposed rule by the ONC will add imaging requirements for EHR certification, aiming to improve access to medical images by 2028. The rule modifies existing certification criteria, including transitions of care and API access, to support electronic image exchange.
It addresses ongoing reliance on CDs for image sharing, despite advancements in digital imaging systems, by promoting integration and reducing the need for physical media. These changes are designed to enhance interoperability without affecting existing information blocking rules.
Moving Beyond the Limitations of Traditional Medical Imaging Systems
Imagine a medical imaging system that aligns with the modern approaches like Citizen, Medicai or Pocket Health, all of which prioritize accessibility, cloud integration, and interoperability.
These platforms propose an easy and secure access to imaging data across devices and locations. They integrate directly with EHRs, support remote sharing, and empower patients, healthcare providers, and even third-parties to collaborate seamlessly.
This vision goes beyond mere image storage, transforming the system into an integral part of the healthcare continuum that breaks down barriers to data accessibility and provides smarter, more connected care solutions.
Traditional PACS solutions, while effective in storing imaging data, often create barriers due to their reliance on proprietary formats and their inability to integrate smoothly with other healthcare systems. This has led to data silos, inefficiencies, and a lack of accessibility for patients and providers alike.
By going beyond the limitations of traditional PACS, the future allows imaging data to move beyond a siloed entity. Instead, it becomes an accessible and dynamic part of the broader healthcare ecosystem—supporting clinicians in providing comprehensive care and empowering patients to be active participants in their health journey.
Opportunities and Benefits in Education, Research and Population Health
Beyond the domain of clinical practice, imaging data exchange offers advantages for a broad range of healthcare initiatives, such as population health management, education, and research. Researchers can acquire significant insights into disease progression, treatment outcomes, and predictive analytics by aggregating large-scale imaging information. This can pave the way for novel medicines and diagnostic tools.
Other Challenges and Considerations: Data Security and Privacy
Despite its transformative potential, the journey towards imaging data exchange at scale is fraught with technical, regulatory, and ethical challenges. The most important is the obligation to protect patient privacy and data security while adhering to strict legal frameworks like the Health Insurance Portability and Accountability Act (HIPAA) and General Data Protection Regulation (GDPR). Healthcare institutions must have strong encryption mechanisms, high-granularity access controls, and data anonymization strategies as guardians of sensitive patient information to reduce the risk of unauthorized disclosure and data breaches.
Collaborative Partnerships: A Call To Collectively Drive the Adoption of Interoperable Solutions
To overcome these challenges, collaborative efforts are needed across industry stakeholders, including healthcare providers, technology vendors, regulatory bodies, and patient advocacy groups.
By fostering a culture of innovation, transparency, and accountability, we can collectively drive the adoption of interoperable solutions that empower patients, enhance clinical workflows, and improve healthcare outcomes.




This is a fascinating topic! Medical imaging has indeed come a long way, especially with the integration of AI and advanced data analytics. The ability to offer personalized care through imaging is transforming patient outcomes. For example, MRI and CT scans can now provide more precise data, enabling doctors to create tailored treatment plans that cater to an individual’s unique health profile. It’s amazing how technologies like 3D imaging and digital pathology are helping with early diagnosis, especially for critical conditions like cancer.
I believe the future of personalized medicine is strongly tied to how we continue to innovate in the field of medical imaging. With the rise of machine learning algorithms that can detect anomalies earlier than human eyes, the potential to save lives and improve treatment efficiency is enormous. Looking forward to seeing how this technology evolves further!