The human brain is a complex and fascinating organ, and understanding its workings requires sophisticated tools.
Electroencephalography (EEG) and Magnetic Resonance Imaging (MRI) are powerful neuroimaging techniques that serve distinct purposes. While MRI is renowned for capturing detailed brain structural images, EEG excels at monitoring the brain’s real-time electrical activity.
But what can EEG show that MRI cannot?
Read the article to discover when EEG is preferred over MRI.

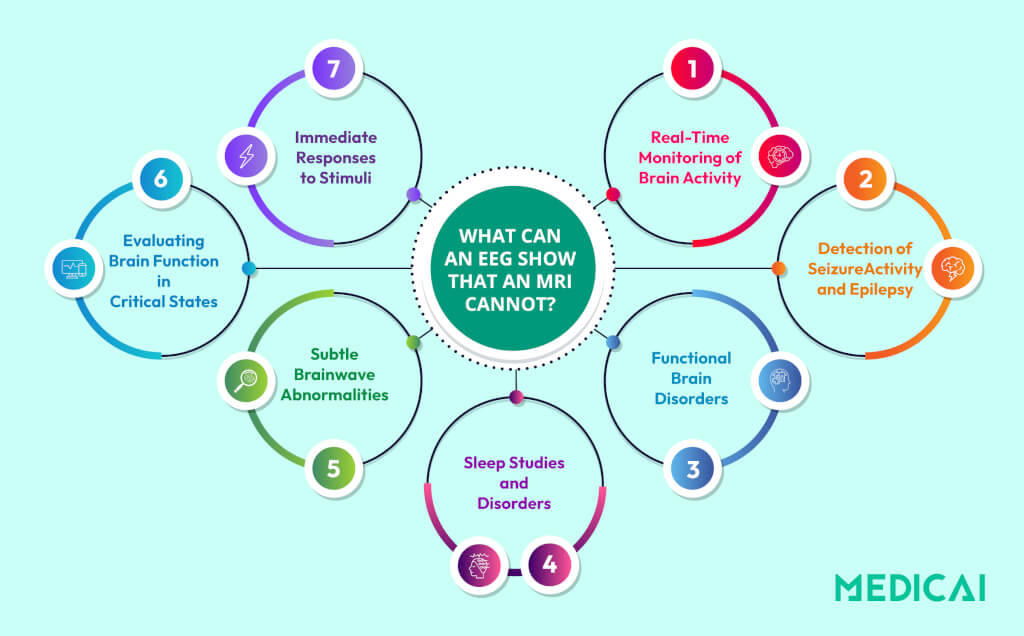
What Can an EEG Show That an MRI Cannot?
EEG (Electroencephalography) and MRI (Magnetic Resonance Imaging) serve distinct purposes when diagnosing and understanding brain health. While MRI focuses on capturing detailed images of the brain’s physical structure, EEG monitors its real-time electrical activity.
This distinction allows EEG to reveal aspects of brain function that MRI cannot. Let’s explore what EEG uniquely offers.
Medicai’s cloud-based PACS infrastructure can securely store EEG and MRI data, making it easily accessible for doctors and patients.

Real-Time Monitoring of Brain Activity
One of the most significant advantages of EEG is its ability to capture the brain’s electrical activity in real time. EEG records brainwave patterns by placing electrodes on the scalp, providing a live window into how the brain functions at any moment.
Real-time monitoring is crucial for understanding transient events such as seizures, cognitive responses, or brain activity during sleep. For example, an EEG can pinpoint the onset and spread of abnormal electrical discharges during a seizure.
On the other hand, MRI excels at static imaging, providing a snapshot of the brain’s physical structure at a single moment. Functional MRI (fMRI) can infer brain activity through blood flow changes, but it lacks the speed and precision to track rapid changes in neural activity.
Detection of Seizure Activity and Epilepsy
EEG is the gold standard for diagnosing epilepsy and other seizure disorders. It detects abnormal electrical discharges in the brain that indicate seizure activity. It works incredibly, even in cases where no structural abnormalities are visible.
Many seizure disorders, such as idiopathic epilepsy, do not have an identifiable structural cause. EEG can still detect the irregular brainwaves characteristic of these conditions. It aids in diagnosis and treatment planning.
MRI can identify structural issues, such as brain tumors, lesions, or scar tissue, that might cause seizures. However, it cannot detect the electrical activity underlying the seizures themselves. The cost of an MRI depends on which part of the body is under investigation.
Functional Brain Disorders
Unlike MRI, which focuses on the brain’s physical structure, EEG is ideal for assessing functional disorders. It includes conditions where the brain’s electrical activity, rather than anatomy, is the primary concern.
Functional neurological disorders, encephalopathy, and certain types of migraines often stem from abnormal brain function. EEG can reveal subtle irregularities in brainwave patterns that are not associated with visible structural damage.
MRI is excellent for detecting tumors, strokes, or malformations. However, it cannot capture issues rooted in how the brain functions in real-time.

Sleep Studies and Disorders
EEG is an essential tool in sleep medicine. It records brain activity during different stages of sleep, such as REM (rapid eye movement) and non-REM sleep. It provides insights into sleep architecture and diagnosing disorders.
Sleep disorders like sleep apnea, insomnia, narcolepsy, and parasomnias often involve disruptions in brain activity. EEG can identify these disruptions and map their timing and intensity across sleep cycles.
However, MRI provides no functional information about sleep states or the transitions between them. So, It cannot diagnose sleep-related brain activity disorders.
Subtle Brainwave Abnormalities
EEG can detect minute abnormalities in brainwave activity that might indicate early-stage neurological conditions or mild traumatic brain injuries (mTBI). These functional changes often occur before structural damage becomes evident.
Early detection of these issues can lead to timely intervention and prevent the progression of a condition.
On the other hand, MRI is limited to identifying structural changes and cannot detect subtle functional abnormalities unless they result in visible damage.
For example, athletes recovering from concussions may have normal MRI results. However, EEG could reveal lingering abnormalities in brainwave patterns, signaling incomplete recovery.
Evaluating Brain Function in Critical States
EEG is often used in critical care settings to assess brain function in patients who are comatose or suspected of brain death. It measures electrical activity to determine whether the brain is still active.
While MRI can show structural damage that might lead to coma, it cannot measure ongoing brain activity.
Immediate Responses to Stimuli
EEG can measure the brain’s real-time responses to external stimuli through evoked potentials like light, sound, or touch. These tests are especially useful for evaluating sensory processing and certain forms of neuropathy.
For example, visual evoked potentials recorded via EEG are used to detect optic nerve damage in multiple sclerosis patients.
However, MRI cannot capture these rapid, real-time functional changes.
Differences Between EEG and MRI
Here’s an in-depth look at the key distinctions between EEG and MRI.
Function vs. Structure
EEG monitors the brain’s real-time electrical activity by placing electrodes on the scalp. It captures brainwave patterns like normal rhythms (alpha, beta, delta) and abnormalities such as seizures or unusual slow-wave activity.
It makes EEG indispensable for diagnosing conditions like epilepsy, sleep disorders, and encephalopathy.
MRI provides high-resolution images of the brain’s structure. It is ideal for identifying physical abnormalities such as tumors, brain injuries, inflammation, and vascular issues.
MRI identifies structural changes related to neurological symptoms, such as detecting the size and location of a brain tumor, which helps with surgical or radiation planning. However, it does not show real-time brain function.
In short, EEG measures function, while MRI examines form—both are essential but address different diagnostic questions.
Temporal vs. Spatial Resolution
EEG boasts exceptional temporal resolution, capturing changes in brain activity within milliseconds. This is crucial for observing fast, transient events, such as seizures, brain responses to stimuli, or changes during cognitive tasks.
However, EEG has relatively low spatial resolution because electrical signals must pass through the skull and scalp, distorting their origin.
MRI provides unmatched spatial resolution, producing highly detailed images of the brain’s structures. It can identify minute changes, such as micro hemorrhages, cortical thinning, or small lesions, which are critical in conditions like stroke, multiple sclerosis, or Alzheimer’s disease.
However, MRI cannot match the millisecond-level precision of EEG in tracking rapid neural activity.
Portability and Accessibility
EEG systems are affordable and portable, making them ideal for outpatient clinics, bedside monitoring in hospitals, and home-based studies. They are also simpler to operate and can be set up relatively quickly.
EEG is also cost-effective, especially compared to MRI, and does not require the same infrastructure or specialized personnel.
MRI requires specialized facilities, including a large scanner, a shielded room, and skilled technicians. This makes it more expensive than EEG, limiting availability to hospitals and larger diagnostic centers. However, the cost of an MRI also depends on other factors like insurance coverage and even the geographic location of the facility.
Besides, the bulky equipment and the need for a controlled environment make MRI impractical for portable use or long-term monitoring. Also, due to the technology and infrastructure involved, costs associated with MRI scans are higher.
| Feature | EEG | MRI |
| Primary Focus | Electrical activity (function) | Structural imaging (form) |
| Temporal Resolution | Millisecond-level precision | Seconds to minutes |
| Spatial Resolution | Limited | High precision |
| Portability | Portable, can be used bedside | Requires a fixed, controlled setup |
| Cost | Lower, cost-effective | Higher, resource-intensive |
When is EEG Preferred Over MRI?
EEG is often favored over MRI when monitoring the brain’s electrical activity, which is crucial for understanding a patient’s condition.
Epilepsy and Seizure Disorders
EEG is preferred for diagnosing and managing epilepsy because it records brain activity. It captures the abnormal electrical discharges that characterize seizures, even when these events occur intermittently.
EEG helps clinicians classify seizures as focal (originating from a specific brain area) or generalized (affecting the entire brain). This information is vital for treatment selection and surgical eligibility.
Sleep Disorders
EEG is a key part of polysomnography, a sleep study that monitors brain activity and other functions like oxygen levels and heart rate. It is important for diagnosing sleep disorders such as:
- Sleep Apnea
- Narcolepsy
- REM Sleep Behavior Disorder
Monitoring Brain Activity During Surgery
EEG is widely used in neurosurgical procedures to monitor brain activity in real-time, ensuring that vital areas of the brain are not damaged during surgery.
During surgeries such as tumor resections or epilepsy surgeries, EEG provides immediate feedback about brain function. This ensures surgeons avoid damaging critical regions responsible for movement, speech, or other essential functions.
MRI cannot be used intraoperatively due to its lack of portability and inability to provide real-time functional feedback during the procedure.
Assessment of Coma and Altered Mental States
EEGs help evaluate patients in comas or with altered levels of consciousness. It can detect residual brain activity, distinguishing between patients with severe brain damage and those who may recover.
It can also identify patterns like burst suppression, indicative of poor prognosis.
MRI can show structural damage but cannot provide information about ongoing brain function.
Neurodevelopmental Disorders
EEG is used to assess neurodevelopmental disorders by analyzing abnormal brainwave activity. It identifies atypical electrical patterns linked to sensory processing and communication issues in children with autism and increased theta wave activity associated with attention deficits.
MRI is not well-suited for evaluating functional aspects of neurodevelopmental disorders, as it focuses on structural changes rather than brain activity.
Combining EEG and MRI
EEG and MRI together provide a comprehensive approach to understanding brain function, leveraging the strengths of each technique.
- Complementary Measurement Techniques: EEG offers real-time insights into neuronal activity with millisecond precision, while MRI captures detailed structural and functional information with millimeter accuracy. Together, they bridge the gap between timing and location.
- Overcoming Limitations: EEG’s high temporal resolution complements MRI’s superior spatial resolution, allowing a fuller understanding of dynamic brain processes.
- Insights into Neural Networks: The combined approach reveals how brain regions communicate, offering a clearer picture of neural connectivity than either modality alone.
- Clinical Applications: In epilepsy, EEG pinpoints seizure activity, and MRI identifies structural abnormalities, improving localization for surgery. This synergy is also valuable in stroke recovery and coma evaluations.
- Research Applications: Integrated EEG-fMRI studies explore attention, memory, and decision-making by correlating rapid brain activity with its precise anatomical origins.
- Improved Experimental Consistency: Simultaneous acquisition ensures consistent data collection, enhancing reliability and accuracy in both clinical and research settings.
Combining EEG and MRI for Specific Medical Conditions
Here are the key conditions where the EEG and MRI combo is particularly beneficial.
- Epilepsy- Seizure Localization: Let’s compare EEG vs MRI for seizures. EEG pinpoints seizure activity, while MRI identifies structural causes like tumors or malformations.
- Brain Tumors- Seizure Risk Assessment: EEG detects electrical abnormalities near tumors, while MRI maps the tumor’s size and location, aiding in risk evaluation and treatment planning.
- Neurodevelopmental Disorders-Autism and ADHD: EEG identifies atypical electrical activity, while MRI highlights structural differences, offering insights into brain function and anatomy.
- Traumatic Brain Injury (TBI) – Comprehensive Evaluation: EEG detects post-traumatic seizures, and MRI reveals structural damage like contusions or hemorrhages, providing a complete picture of injury impact.
- Sleep Disorders: EEG monitors brain activity to diagnose conditions like sleep apnea or narcolepsy, while MRI rules out structural abnormalities affecting sleep.
- Coma and Altered Consciousness – Prognostic Insights: EEG assesses brain activity levels in comatose patients, while MRI identifies underlying causes like strokes or tumors.
- Inflammatory Diseases – Multiple Sclerosis (MS): EEG monitors functional changes, while MRI visualizes demyelinating lesions, helping track disease progression and treatment response.

MRI Scan Normal vs Abnormal Brain MRI
The distinction between a normal and an abnormal brain MRI hinges on the presence of visible structural changes, signal abnormalities, or deviations from expected anatomy.
Normal Brain MRI Findings
A normal brain MRI is often described as “unremarkable” or “normal for patient age.” It shows a healthy anatomy and expected features, including:
- Clear Differentiation: A distinct and sharp line between the gray matter (the outer layer where processing occurs) and the white matter (the tracts connecting different brain regions).
- Symmetry and Alignment: The structures of the brain and the spaces containing cerebrospinal fluid (the ventricles) appear symmetrical and centered along the midline.
- Absence of Masses: No evidence of tumors, cysts, abscesses, or other space-occupying lesions.
- Normal Signal Intensity: Brain tissues (gray matter, white matter, and fluid) produce predictable signals across different MRI sequences (T1, T2, FLAIR).
- Vascular Health: Blood vessels are free of significant blockages or abnormal formations (like large aneurysms).
Note: A normal brain MRI may still contain incidental findings like small, harmless arachnoid cysts or minor age-related changes that are not clinically significant.
Abnormal Brain MRI Findings
An abnormal MRI shows structural changes or tissue abnormalities that may indicate a neurological disease or injury. The type of abnormality is key to diagnosis.
| Abnormal Finding | Potential Causes | Key Characteristics on MRI |
| Masses/Lesions | Tumors (benign or malignant), Metastases (cancer spread), Abscesses (infection). | An area of tissue that is not normal brain tissue; often appears as a lump or ring-enhancing structure, sometimes with surrounding edema (swelling). |
| Ischemic Changes (Stroke) | Interrupted blood flow due to a blockage (ischemic stroke). | An area of brain tissue death (infarct) that appears bright on specific sequences (like DWI) in the acute phase. |
| Hemorrhage (Bleeding) | Trauma, high blood pressure, ruptured aneurysm (hemorrhagic stroke). | Collections of blood that appear as distinct signal changes depending on the age of the bleed. |
| White Matter Hyperintensities (WMH) | Small vessel disease (e.g., from hypertension or diabetes), Multiple Sclerosis (MS). | Bright spots, often around the ventricles, indicating damaged nerve fibers. In MS, these lesions often have a specific location and shape (e.g., “Dawson’s fingers”). |
| Atrophy | Alzheimer’s disease, Frontotemporal Dementia, other neurodegenerative diseases, or advanced aging. | Loss of brain volume, resulting in an enlargement of the fluid-filled spaces (ventricles and sulci) in specific regions (e.g., medial temporal lobe atrophy in Alzheimer’s). |
| Inflammation/Infection | Collections of blood appear as distinct signal changes depending on the age of the bleed. | Meningitis, Encephalitis, and Autoimmune conditions. |

Normal Brain MRI but Abnormal EEG
The combination of a normal MRI and an abnormal EEG is often a key diagnostic finding that strongly suggests a functional disorder over a structural one.
This finding, “normal brain MRI but abnormal EEG,” is very common and significant in neurological evaluation. It indicates that while the brain’s structure (anatomy) appears normal, its function (electrical activity) is abnormal.
| Condition | Explanation of the Abnormal EEG |
| Epilepsy (Seizures) | This is the most common reason for this finding. An EEG is critical for diagnosing epilepsy because it can capture epileptiform discharges (spikes or sharp waves), even between seizures (interictally). Many forms of epilepsy, particularly idiopathic generalized epilepsies, have no structural cause, leading to a normal MRI. |
| Metabolic/Toxic Encephalopathies | These involve physical, real problems with the nervous system that are not due to a structural abnormality. The EEG may show patterns that do not correlate with classic seizure activity. |
| Functional Neurological Disorders | These involve problems with the functioning of the nervous system, which are physical and real, but are not due to a structural abnormality. The EEG may show patterns that do not correlate with classic seizure activity. |
| Early Stages of Certain Dementias | In the early course of some neurodegenerative diseases (like Alzheimer’s disease), the MRI may be normal, but the EEG can begin to show mild generalized slowing as brain function declines. |
| Mild Traumatic Brain Injury (mTBI/Concussion) | Following a concussion, the EEG may show subtle functional abnormalities or slowing, even if the structural MRI remains entirely normal. |
The Future of EEG and MRI Integration
Let’s look at some key areas of development in EEG-fMRI technology:
- Enhanced Data Acquisition Techniques: Future developments aim to refine simultaneous EEG-fMRI recording by minimizing artifacts caused by the MRI environment. Innovations like advanced EEG caps designed specifically for MRI compatibility will improve data clarity while maintaining patient safety.
- Advanced Analysis Methods: Integrating machine learning and AI into EEG-fMRI analysis will help researchers uncover complex patterns and correlations between electrical and hemodynamic activity. It offers deeper insights into brain connectivity and state transitions.
- High-Resolution Imaging: Laminar fMRI, a high-resolution imaging technique, will enable detailed mapping of cortical layers alongside EEG signals. This advancement will allow researchers to study the contributions of different cortical layers to brain function and connectivity.
- Exploration of Non-BOLD Signals: Future research may enhance fMRI by incorporating non-BOLD hemodynamic markers like cerebrospinal fluid (CSF) flow. When combined with EEG data, this could deepen our understanding of brain dynamics beyond conventional BOLD responses.
- Real-Time Applications: Dynamic monitoring and real-time EEG-fMRI feedback could transform clinical and cognitive training settings.
- Expanded Clinical Applications: As the technology matures, EEG-fMRI will likely become a standard diagnostic tool for a broader range of neurological conditions, such as mood disorders, neurodegenerative diseases, and sleep disorders.
EEG vs MRI vs CT Scan: Picking the Right Modality
Why three tools?
Because each tells a different‐yet‐complementary story about the brain. EEG captures electrical chatter in real time; MRI maps soft-tissue anatomy in exquisite detail; CT delivers rapid structural snapshots—especially of bone and acute bleeding.
Understanding their strengths (and blind spots) helps clinicians order the right test first and avoid costly delays.
| Feature | EEG | MRI | CT Scan |
|---|---|---|---|
| Primary insight | Ongoing electrical activity (function) | High-resolution soft-tissue anatomy ± blood-flow changes (fMRI) | Density differences—bone, blood, calcification (structure) |
| Temporal resolution | Milliseconds (best) | Seconds to minutes | < 1 sec per slice, but not live activity |
| Spatial resolution | Centimeters—source estimation only | Sub-millimeter (best) | ~0.5–1 mm for bone; soft tissue moderate |
| Radiation exposure | None | None | Ionizing X-ray dose |
| Scan speed & availability | Setup 10–20 min; portable | 15–60 min; fixed suite | 2–5 min; widely available, ED staple |
| Best-fit clinical questions | • Seizure focus • Coma prognostication • Sleep architecture | • Tumors, demyelination, ischemia • Surgical planning • Sub-acute stroke penumbra | • Acute head trauma • Intracranial hemorrhage • Fractures & calcifications |
| Key limitations | Poor localization; artifacts | Cost, motion sensitivity, claustrophobia | Radiation; limited soft-tissue contrast |
Conclusion
The integration of EEG and MRI represents a groundbreaking advancement in neuroimaging, offering unparalleled insights into brain function and structure. Combining real-time electrical activity monitoring with anatomical imaging improves diagnostic precision and treatment planning for neurological conditions.
At Medicai, we are committed to leveraging cutting-edge solutions like EEG and MRI to provide innovative, patient-centered care and advance the future of neurodiagnostics.






