Every child deserves the right diagnosis at the right time. However, pediatric radiologists are scarce, leading to long waits or journeys for families seeking expert care.
Pediatric teleradiology changes that story.
Pediatric teleradiology connects hospitals and clinics with remote pediatric radiologists, delivering faster, expert interpretations of children’s scans. It provides accurate diagnoses without requiring families to travel, bridging the gap in access to subspecialty care worldwide.
Let’s uncover why pediatric teleradiology matters, the hurdles it faces, and how new solutions are reshaping children’s healthcare.

The Global Gap in Pediatric Radiology Access
Access to pediatric radiologists is far from equal. In many parts of the world, the number of specialists is alarmingly low. Some Sub-Saharan African countries, for example, have no pediatric radiologists working in public service at all.
Even in wealthier regions, subspecialists are clustered in major cities, leaving community hospitals and rural clinics without immediate support.
The impact is profound. Conditions like tuberculosis, pneumonia, congenital heart defects, or childhood cancers require precise imaging interpretation. Without pediatric expertise, misdiagnoses or delayed diagnoses are more likely.
For a child with pneumonia in an HIV-prevalent region, that delay could mean the difference between recovery and serious complications.
Families are often forced to travel long distances to specialized hospitals, adding financial strain and emotional stress.
What Is Pediatric Teleradiology?
Pediatric teleradiology is the remote interpretation of medical images in children by subspecialty-trained radiologists. Children’s imaging poses unique challenges; what appears normal in a growing child may indicate disease, and adult-focused interpretations can overlook subtle pediatric findings.
Unlike general teleradiology, which often covers routine chest or orthopedic scans, pediatric teleradiology emphasizes growth-related conditions, congenital abnormalities, and illnesses like pneumonia or tuberculosis that appear differently in children.
It also pays closer attention to minimizing radiation exposure and using age-appropriate imaging protocols.
Research on pediatric teleradiology demonstrates its feasibility and increasing significance, particularly in low-resource settings for diagnosing childhood diseases such as tuberculosis and pneumonia. Projects collected data on diagnostic accuracy, turnaround times, image quality, and patient management impact.
Emerging research is exploring point-of-care ultrasound telereading for conditions such as pediatric TB and neonatal brain imaging, expanding teleradiology beyond traditional X-rays. These findings confirm that, despite challenges, pediatric teleradiology positively impacts children’s healthcare worldwide.

How Pediatric Teleradiology Works
At its core, pediatric teleradiology is simple: capture the image locally, interpret it remotely, and deliver the report back quickly. But when applied to children’s care, every step matters.
- Image Capture: A child undergoes an X-ray, CT, MRI, or ultrasound at a local hospital or clinic. Pediatric-friendly protocols like lower radiation doses are often used.
- Upload to Cloud PACS: Instead of relying on hard-copy films or low-quality JPEGs, digital images are securely uploaded in DICOM format to a cloud-based PACS for pediatric use. This ensures diagnostic quality is preserved.
- Remote Review by Pediatric Radiologist: A subspecialist receives the scan, interprets it, and notes findings specific to children’s conditions, from subtle fractures to early signs of TB or congenital defects.
- Report Transmission: A structured report is sent back to the referring physician. Turnaround times can range from minutes to a few hours, depending on the urgency.
- Care Team Action: Pediatricians, surgeons, or emergency doctors act on the findings immediately, ensuring treatment isn’t delayed.
This workflow turns a local clinic into a point of access for global expertise. With platforms like Medicai, the process becomes faster, more secure, and better integrated into pediatric care systems worldwide.
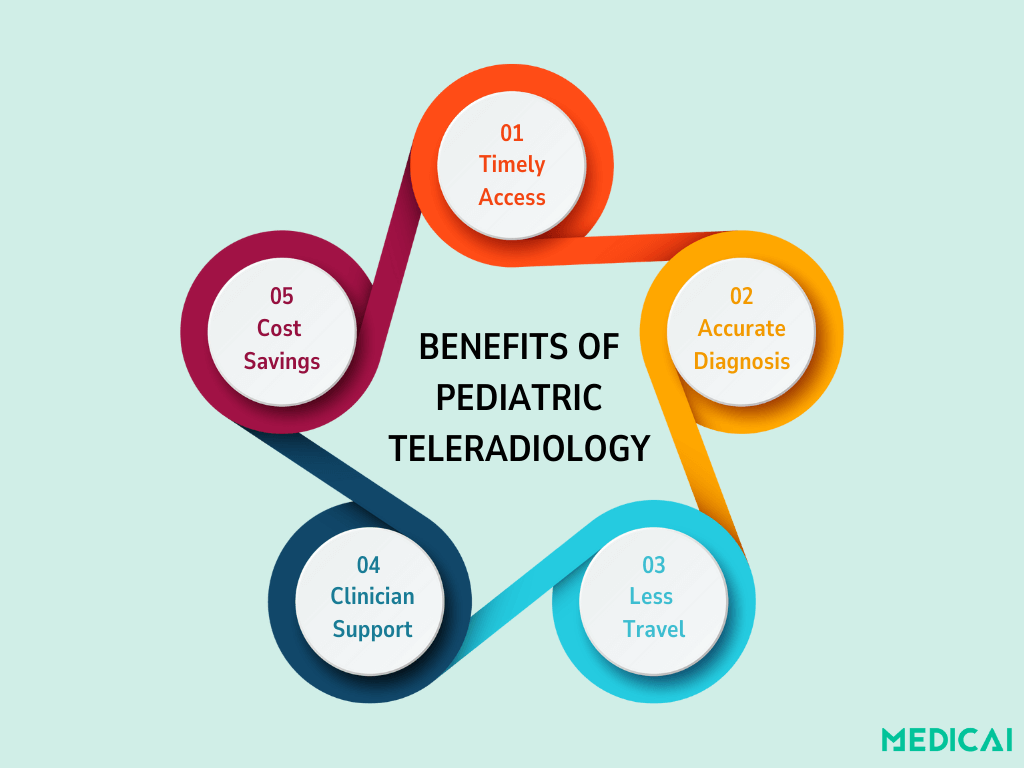
Key Benefits of Pediatric Teleradiology
Pediatric teleradiology is a vital resource for children, families, and medical teams. When done well, the benefits reach far beyond the imaging room.
- Timely access to expertise: Children in rural or underserved areas can have their scans read by pediatric specialists within hours, instead of waiting days for transfer or referrals.
- Improved diagnostic accuracy: Subtle signs of diseases like TB, pneumonia, or congenital heart conditions are easier to spot with pediatric-trained radiologists, reducing the risk of misdiagnosis.
- Less travel for families: Parents don’t need to take their children across long distances to reach specialized hospitals. Expert care comes to them through the cloud.
- Support for local clinicians: Pediatric teleradiology doubles as a teaching tool, helping general doctors or radiographers learn from subspecialist reports and feedback.
- Cost-effectiveness: Hospitals avoid unnecessary transfers and duplicate tests, while families save on time and expenses. For low-resource settings, this can mean the difference between access and abandonment of care.
Challenges and Barriers in Pediatric Teleradiology
While the promise of pediatric teleradiology is strong, several real-world barriers stand in the way of success.
Image Quality Issues
In many projects, hard-copy films were photographed and emailed as JPEGs. Poor exposure, rotation, and artifacts often made scans difficult to interpret. Without consistent quality, even expert radiologists face limits.
Moving to digital X-ray and direct DICOM uploads via cloud PACS preserves diagnostic detail. AI-driven quality checks can flag underexposed or mispositioned images before they reach the radiologist.
Bandwidth And Connectivity
Low internet speeds and high data costs remain major challenges in low-resource settings. Compressing images helps, but excessive compression can compromise diagnostic value.
Optimized compression algorithms achieve smaller file sizes while maintaining quality, and offline-first workflows sync when internet access improves, reducing reliance on high bandwidth.
Language And Communication Gaps
Radiologists and local physicians may struggle to share findings clearly, leading to misinterpretation of reports.
Structured reporting templates and multilingual support tools may ensure clarity, while integrated chat and teleconsultation features can foster real-time collaboration between clinicians and radiologists.
Sustainability
Many pilot programs work at first but stall when funding ends. Without long-term planning, governance, and trained staff, services fade away.
Cloud-based platforms like Medicai with pay-per-use pricing models, combined with local training programs and academic “buddy systems,” can create long-term sustainability beyond the pilot stage.

Future of Pediatric Teleradiology
The next chapter of pediatric teleradiology is about moving from improvised fixes to sustainable, technology-driven systems.
Cloud-Native Platforms.
Instead of relying on emailed JPEGs, hospitals can now upload full-quality DICOM images to secure AI-driven cloud PACS. This preserves diagnostic detail and ensures reports can be turned around quickly, even across borders.
Ai Support
Artificial intelligence is emerging as a safety net for pediatric imaging. From flagging signs of pneumonia or TB on chest X-rays to alerting doctors about poor-quality scans, AI can speed up triage and help radiologists focus on the most urgent cases.
Point-Of-Care Ultrasound
Ultrasound is safe, portable, and especially suited for children. Recent research shows that even non-radiologists can capture standardized sweeps, which can then be sent to specialists for review.
This opens new doors for diagnosing conditions like pneumonia or neonatal brain injury in low-resource clinics.
Global Partnerships
Universities, NGOs, and children’s hospitals are forming “buddy systems” to share expertise and training. These partnerships strengthen local capacity while ensuring children get timely access to subspecialists.
Conclusion
Pediatric teleradiology is more than a technological solution—it’s a bridge to equity in children’s healthcare. Connecting local clinics with global pediatric radiologists, it ensures faster diagnoses, accurate reports, and timely treatment for young patients everywhere.
Cloud-based platforms like Medicai and AI-driven tools are paving the way forward. Our solutions make pediatric imaging practical and accessible for every child, regardless of the setting.



